Antioxidant Supplements Unlikely to Boost Men’s Fertility
Antioxidant therapy had little effect on sperm quantity, quality, shape or motility.
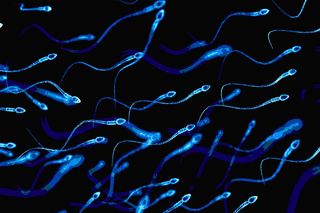
A new, large-scale study is casting doubt on previous studies that suggested antioxidant supplements can improve men’s fertility, finding instead no statistically significant improvement in sperm quality among infertile men who underwent three months of antioxidant therapy.
The study, which was conducted across eight American fertility centers, involved 174 couples of whom the male partners suffered from male factor infertility, that is, abnormal sperm quantity, shape, mobility or DNA quality.
The researchers tested sperm samples for these characteristics at the beginning of the study as well as at the end. During the three months between, one randomly selected group of men took daily antioxidant supplements (vitamins C, D3 and E, as well as folic acid, zinc, selenium and L-carnitine), while the other group took a daily placebo.
Natural antioxidants, including vitamins C and E, are found in semen ostensibly as protection against the activity of free radicals and oxidative stress, which has been linked to DNA degradation. Several studies have shown that antioxidant levels are lower in the semen of infertile than in fertile men — thus, the rationale for antioxidant therapy. And since men’s bodies produce, mature and transport new sperm on a roughly 74-day cycle, explained Dr Anne Steiner, of the University of North Carolina at Chapel Hill, USA, any improvement related to antioxidant supplementation could be expected to show up within the study’s three-month timeline.
But at the end of 90 days, researchers found overall only marginal differences in sperm quantity between the antioxidant group and the placebo group, and negligible differences in shape, mobility and DNA quality. When the results were examined by type of sperm abnormality — for example, men whose infertility is due to low sperm count, or to poor DNA quality — the researchers also found no significant change effected by the antioxidant supplements.
The team also took into account the rate of natural conception during the trial period. They found a marginal difference in pregnancy rates among partners of men in the antioxidant group (10.5%) and men in the placebo group (9.1%).
“The results do not support the empiric use of antioxidant therapy for male factor infertility in couples trying to conceive naturally,” Steiner and colleagues concluded. Steiner recently presented their findings at the annual meeting of the European Society of Human Reproduction and Embryology in Barcelona, Spain.
Or even, perhaps, in couples trying to conceive with assistance; pregnancy rates held steady even after male partners continued receiving antioxidant and placebo therapy for six months, while all female partners received three cycles of clomiphene and underwent intrauterine insemination (IUI).
In previous studies, antioxidants have been linked to improved sperm quality. However, the researchers pointed out these studies were limited by few participants, a lack of diversity among participants, variations in the antioxidants prescribed, and outcome measures.
Related


The History of Birth Control in India Was Never About Empowerment