
Covid19 Drug Dexamethasone May Have ‘Little to No Benefit’ For Women, Suggests Research
“It’s possible the mainstay therapy for severe Covid19 that we’re giving everybody is only benefiting half the population. This is a big problem.”

New research has found that dexamethasone, a steroid widely used as the main treatment for severe Covid19 infections, may work for male patients but have “little to no benefit” for female patients. The multidisciplinary study, led by researchers at the University of Calgary, Canada, was published in Nature Medicine on Monday.
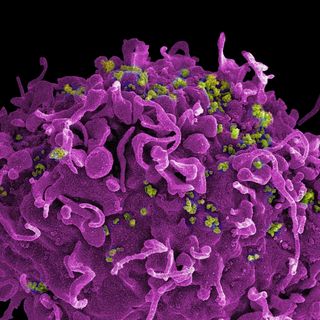
Dexamethasone is a corticosteroid (steroid hormone) that reduces inflammation. For people with severe Covid19 infections, their bodies’ immune systems go into overdrive and attack their own cells — leading to fatal outcomes in many cases. According to research, dexamethasone calms this immune response. Thus, it quickly became the treatment of choice for severe cases of Covid19 around the world.
Medical practitioners began using steroids to treat severe infections based on data about their impact in reducing mortality. But there was little research on how effective the drugs were for Covid19 infections in particular, and how effective they were in reducing mortality. Exactly what steroids did on a cellular level also remained relatively unclear. Researchers also didn’t understand how the Covid19 virus itself interacted with immune cells on a cellular level.
“To be able to develop new treatments, we wanted to study how different people respond to SARS-CoV2 infection and how different immune responses dictate the severity of their disease,” Jeff Biernaskie, professor, Comparative Biology and Experimental Medicine in the Faculty of Veterinary Medicine (UCVM) and author of the study, told Science Daily.
What they found was disquieting. Having analyzed data from all ICU admissions during the pandemic, the researchers found that dexamethasone only reduced the number of male patients dying but had no effect on the female population in Alberta.
Researchers collected blood samples from patients admitted with severe respiratory distress to analyze their immune cells at different stages of the disease. With most viral infections, proteins called interferons (IFNs) signal neutrophils — a white blood cell and an important part of the immune system — to circulate. Covid19 was “associated with the expansion of distinct neutrophil states characterized by interferon (IFN)… signaling,” the paper noted.
Related on The Swaddle:
WHO Backs Dexamethasone for Covid19, But on What Basis?
“Surviving SARS-CoV-2 depends on striking a temporal balance between inciting viral clearance immune programs during the early stage and subsequently restraining those same programs at later stages to limit immunity-induced damage,” the paper added.
Here is where dexamethasone enters the picture. Administering it too early may have a negative impact because it would interfere with the virus-clearing stage of the immune response. But in critical patients, it could restrain immune activity from damaging healthy cells. In more technical terms, dexamethasone was found to alter the circulation of IFN neutrophils. But here is the catch: male patients had more IFN active neutrophils, thus making the dexamethasone more effective for them.
“What we found was that specifically in males, we see an exaggerated neutrophil interferon response, that is significantly restrained when a patient is given dexamethasone… But with females, relative to males, [the] neutrophil interferon response was much more tempered, so dexamethasone had little effect,” said Biernaskie.
The findings point to a sex bias in the way that dexamethasone works. Researchers call for individualized therapies, or precision medicine, to ensure that diseases like Covid19 aren’t treated with such ablanket approach.
“Currently, it’s possible the mainstay therapy for severe Covid19 that we’re giving everybody is only benefiting half the population. This is a big problem,” said Bryan Yipp, MD, associate professor, Department of Critical Care Medicine, Cumming School of Medicine, and author of the present study.
A previous report by a research collaboration noted how the lack of sex-disaggregated information on how Covid19 affects men and women differently has implications on several levels. “Aside from a lack of infection and mortality numbers broken down by sex, a lack of research into sex differences in the experience and effects of Covid19 could have an adverse impact on pandemic treatment, recovery, and vaccination programs,” wrote Devrupa Rakshit for The Swaddle.
The research thus points to yet more evidence of how medicine is ingrained with a neutrality bias that assumes male bodies are the standard “neutral” bodies to conduct research on. As a result, research neglects to account for sex differences, often leading to fatal consequences for women and gender minorities. The Covid19 experience is the latest chapter in this long and ancient story, and medical research is just now waking up to the consequences.
Rohitha Naraharisetty is a Senior Associate Editor at The Swaddle. She writes about the intersection of gender, caste, social movements, and pop culture. She can be found on Instagram at @rohitha_97 or on Twitter at @romimacaronii.
Related

A Woman’s Immune System ‘Naturally’ Cured Her of HIV
