
Vaccines Work Better In Some Parts of the World Than Others
Vaccines are safe, but less effective in the developing world. Why?
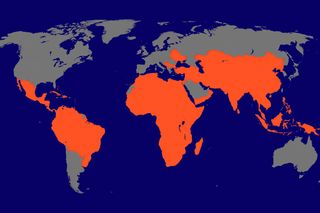
Scientists and physicians have for years pondered a medical mystery: Why do vaccines work better in some parts of the world than in others? A new study, led in part by University of Minnesota Medical School researcher Tim Schacker, MD, contributes to knowledge about why vaccines given in the developing world often are less effective than in the developed world.
The study, to be published in the Journal of Clinical Investigation, finds that diseases common in the developing world might be a culprit. For example, malaria, tuberculosis and infections caused by parasites may damage lymph node structures that are crucial to developing immunity after a vaccine.
“One of the unanswered questions in vaccine research is why some vaccines work well in the developed world but very poorly in the developing world–especially in more tropical climates. We wanted to know whether environmental factors or pervasive infections in developing areas were making vaccines less effective,” says Schacker, a professor of infectious diseases and international medicine and director of the Program in HIV Medicine at the University of Minnesota. “Our research suggests that having certain diseases does affect the body’s ability to prompt immune protection after a vaccine.”
For the study, researchers evaluated groups of people from Uganda and the United States. They found that the Ugandans have significantly higher levels of inflammation in their bodies and a depleted supply of protective T cells. Their secondary lymph nodes, where vaccine responses happen, had fibrosis or thickening and scarring from the inflammation.
Schacker’s research uncovered significant differences in the lymphoid anatomy between subjects in Uganda and the United States. Every Ugandan participant showed evidence of differences in the anatomy of their secondary lymph nodes compared to participants in the United States. These differences include fibrosis, increased immune activation and other anatomy changes that would be considered abnormal in the United States.
With this evidence in hand, researchers then explored whether such differences hindered the Ugandans’ response to vaccinations. They gave Ugandans a yellow fever vaccination and monitored them for 60 weeks, seeking to determine whether their lymphoid abnormalities were associated with immune dysfunction. In addition, they found correlations between the Ugandans’ limited antibody response to the vaccine and the amount of damage from inflammation and fibrosis in the lymph nodes. “We showed that the degree to which these tissues were damaged by inflammation was significantly associated with the response to a vaccine,” Schacker says. “This suggests that common infections in the developing world may be an important limiting factor in the development of immune response to a vaccine.”
“We believe that these data have important implications for how vaccines are designed and tested for infections that greatly impact the developing world,” he adds. “This is especially true of vaccines for HIV, malaria, and TB–diseases that are responsible for the greatest number of deaths.”
Related


Are You Remembering Your Childhood Correctly?
