
Everything You Need to Know About Chlamydia
Blink and you might miss it.
Chlamydia is a common sexually transmitted infection (STI) that can affect women and men of all age-groups. Often, those who have chlamydia may not even know that they have the infection because it will never develop into noticeable or lasting signs or symptoms. That said, treatment for chlamydia isn’t difficult once you know you have it. If left untreated, however, chlamydia can lead to serious health problems.
What is chlamydia and how is it transmitted?
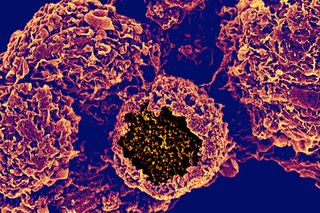
Chlamydia is caused by a bacteria called Chlamydia trachomatis, and is said to be the most common bacterial sexually transmitted infection worldwide. It is an STI, which means you can get it through having unprotected vaginal, anal or oral sex with someone who has the infection.
You can get chlamydia from someone even if there is no penetration, orgasm or ejaculation; it can be passed simply from skin-to-skin contact with infected genitals, or if infected semen or vaginal fluid enters your eye.
However, chlamydia can’t be passed on through casual contact, such as kissing and hugging, or from sharing baths, towels, swimming pools, toilet seats or cutlery.
It can be passed by a pregnant woman to her baby and may lead to newborns developing eye infections (conjunctivitis) and lung infections (pneumonia). But, on noticing these symptoms, doctors will typically prescribe a test for chlamydia and prescribe antibiotics to treat the baby’s infection.
How prevalent is it? Is there a way to avoid it?
According to the World Health Organization (WHO), 500 million new cases of one of four curable STIs (chlamydia, gonorrhoea, syphilis and trichomoniasis) occur each year worldwide.
As per an India-specific, 2017 report, India is home to the world’s greatest burden of infectious diseases, yet information on prevalence rates of chlamydia is scarce. A compilation of 27 small studies on the infection in India suggests it is most prevalent among young women (possibly due to the infection going undiagnosed). However, its prevalence among both genders varies greatly depending on region, and with the sparse data available, a population-wide figure is impossible to arrive at.
Anyone who has sex with someone with a chlamydia infection can catch chlamydia. The risk is greatest for those who have a new sexual partner and don’t use condoms. Using condoms or dental dams (a piece of thin, soft plastic or latex) are the best preventative methods, though they are not guarantees against the infection.
What are the symptoms of chlamydia?
Chlamydia infections are often asymptomatic and, hence, frequently go undiagnosed. Even if signs or symptoms do occur, they usually start one to three weeks after exposure to chlamydia and are often mild and passing, making them easy to overlook.
But some potential chlamydia symptoms to look for include: painful urination, lower abdominal pain, abnormal vaginal discharge or discharge from the penis, painful sexual intercourse, bleeding between periods and after sex in women, and testicular pain in men. If you notice any of these, it’s time to see a doctor.
When chlamydia infections go undiagnosed, they can carry some serious long-term consequences. These are different for men and women. In men, undiagnosed chlamydia can spread to the testicles and epididymis (tubes that carry sperm from the testicles), causing them to become painful and swollen, a condition known as epididymitis. Although it is treatable with antibiotics, there’s a possibility it could affect fertility. It could also cause Sexually Acquired Reactive Arthritis (SARA) (possible in women but more common in men) in which your joints, eyes or urethra become inflamed, usually within the first few weeks after having chlamydia. There’s currently no cure for SARA, but most people get better in a few months. In the meantime, treatment with anti-inflammatory drugs such as ibuprofen can help relieve the symptoms.
In women, chlamydia can spread to the womb, ovaries or Fallopian tubes leading to pelvic inflammatory disease (PID). PID can cause difficulty getting pregnant, or infertility, chronic pelvic pain, and an increased risk of ectopic pregnancy (where a fertilized egg implants itself outside the womb). PID is usually treated with a 2-week course of antibiotics. The risk of experiencing problems such as infertility is lower if it’s treated early, so it’s important to seek medical advice as soon as you notice symptoms of the condition.
How do you get diagnosed?
Screening and diagnosis of chlamydia is relatively simple. Tests include:
For women: A swab of the cervix, which can be done during a routine Pap test.
For men: A swab of the urethra. In some cases, a doctor may also swab the anus.
Another way to get tested for chlamydia is through a urine test.
If you’ve been diagnosed with a chlamydia infection, it’s important that your current sexual partner and any other recent sexual partners be informed, tested and treated to help stop the spread of the infection.
Public health experts advise that people who are sexually active with new and/or multiple partners should be (re)tested for chlamydia every three months.
What is the treatment for chlamydia?
Although chlamydia doesn’t usually cause any symptoms, when it is diagnosed, it can be treated with a short course of antibiotics. You may be given some tablets to take all on one day, or a longer course of capsules to take for a week. Treatment for complications related to an undiagnosed chlamydia infection differ (see above).
Doctors usually recommend not having sex until you and your current sexual partner have finished the treatment. If you had the 1-day course of treatment, you should avoid having sex for a week afterwards.
Can chlamydia be cured?
Chlamydia can be cured with antibiotics. When taken properly, antibiotic treatment will stop the infection and lower your chances of having complications later on. You should not share medication for chlamydia with anyone.
Having chlamydia or having been treated for it in the past provides no immunity against reinfection in the future, though, so one should ideally be tested for the infection after the first time having sex with any new partner.
This is part of our series on sexually transmitted infections.
Related


Coffee Fiends Live More Dangerously Than They Know
