
No One Tells You Fibromyalgia Affects Your Sex Drive; They Should
“I cannot recall being asked about sexual function even once by the slew of doctors.”
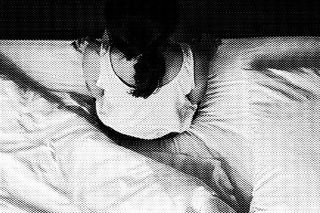
Unopened, shiny, red boxes of condoms that are fast approaching their expiry date.
Guilt and more guilt.
A jolt of pain. Or two.
Extreme nausea. Occasional repulsion.
Willingness to hold and be held. Unwillingness to touch and be touched.
Mostly, though, a bizarre and unprecedented absence of the spark in the loins, of a tingling under the membranes of the skin, of an alacrity to take one’s own clothes off – and then someone else’s – that has plagued my sexual existence for more than half a year.
I am 30 years old, live with my boyfriend, write for a living, and exercise and eat healthier (on most days) than a fitness catalog. Almost all of those conditions are augmented, influenced — and aggravated — by my fibromyalgia.
For the uninitiated, fibro is a chronic pain syndrome whose origins may range from genetics to stress. It’s also characterized by extreme fatigue, cognitive dysfunction (you know, the occasional and completely charming tendency to forget your two-item grocery list by the time you get to the grocery store), sudden bouts of nausea, indigestion, and mood swings, among many (many, many) other indeterminate symptoms. Most of these Wikipedia will tell you. Or a fellow fibro warrior, if you ask nicely enough. What even she (for, it is mostly a ‘she’; 90% of cases, according to US government statistics, are diagnosed in women) will probably hesitate to tell you is that one common symptom is sexual dysfunction.
And while we’re no longer feeling it, we’re sitting quiet and despairing, believing this to be the last of our worries. Who cares whether we come or not when we have the world to save and invisible pain to battle? Who cares, especially since the world never cared much for a woman’s sexuality anyway, give or take a little fibromyalgia?
Losing the erogenous plot
I’m not sure when I started to lose the erogenous plot. I can fuzzily remember a time when my boyfriend and I rolled over each other’s bodies, laughing at our combined libidos and wondered, mock-condescendingly, if other couples past their three-year prime had as much sex on a daily basis. Sex was a part of the equation, equally and equitably shared within the relationship with no basis or necessity for withholding or withdrawal. Until the fibro storm struck – and with it, the inevitable crash-and-burn of all equitability. Suddenly, I could no longer say we defied all clichéd definitions of gendered sex drives because he was doing all the heavy lifting.
There are times when the anti-depressants I am prescribed for fibro will suppress my libido. Then, there are times when, as other fibro-warriors on pan-India WhatsApp support groups tell me, the accompanying mood swings kill sexual appetite. There are also times when you and I, and my partner, can play guessing games at what is causing my sex drive to dim and ebb, and none of us be the wiser. Usually, it’s the third case.
Related on The Swaddle:
At some point, I reached out to a friend with fibro and managed to ask her if she felt the same. “All the time,” she said, preferring to remain anonymous. “Sex was always accompanied by fatigue and listlessness in the beginning. Many a time, there was this involuntary crying that happened after the act. Luckily, my husband understood and was supportive throughout. Exercise and meditation help a lot these days.”
Looking for any kind of guidance
When I first started to panic about this rather new symptom – to add to my ever-growing list of things I (and indeed, most doctors) did not understand about fibro — I turned to the internet. Google throws up a billion and one Reddit threads and medical conjecture about the link between sexual dysfunction (SD) and fibromyalgia (FM), but no one’s prepared to make a sweeping conclusion.
Several studies and expert commentaries speak to this conjecture, however. In 2016, a study conducted by the Mevlana University School of Medicine – which claimed to be the first study conducted to link SD and mood, anxiety and personality disorders in patients with FM – indicated that 50 of the 96 patients surveyed (so, over half) suffered from SD. “The most common SD was lack of sexual desire … and arousal disorder ….”
While the study specified that “pain, rather than a mood disorder, played a greater role in the etiology of SD in patients with FM,” it also concluded that studies on a larger scale were needed to examine SD. Perhaps the line that stayed with me the most was Dr. Randy Fink’s, medical director of the Miami Center of Excellence for Obstetrics and Gynecology. Quoted by Everyday Health, Fink suggests: “Your brain is the biggest, strongest, most sensitive sex organ. When it’s focused on pain, it can’t handle the task of igniting desire.”
I cannot recall being asked about sexual function even once.
Which is it then? A mood thing, or the sheer, stark pain – that causes SD in me (and a statistically large number of other women with fibro)?Findings keep arguing over the root cause, but perhaps what we really need is just a questionnaire that sensitively and empathetically asks women, at the very least, whether they’d like to address their sexual worries post the FM diagnosis?
Dr. Shobhana Mittal, a psychiatrist at CIMBS, Delhi, agrees. “It is important for doctors to remember to ask about sexual dysfunction when treating a female patient on medications that can cause certain sexual side effects.”
Mittal, however, warns of a Catch-22: “When medications like SSRIs, SNRIs and TCAs are given, whether for pain and fatigue — or for depression and anxiety that often accompany these disorders — in 40 to 60% of these cases, the medication itself can cause or worsen sexual dysfunction, like vaginal dryness, decreased libido, and a decreased inability to experience an orgasm. However, if medication is stopped, that could likely worsen the underlying disorder, which causes sexual dysfunction on its own. This is a Catch-22.”
Mittal believes a doctor should take the initiative to “switch you to a different medication, adjust your dose, or suggest techniques to manage the dysfunction — e.g. using lubrication in case of vaginal dryness.”
But I cannot recall being asked about sexual function even once by the slew of cardiologists, pulmonologists, general physicians, pain management specialists, and rheumatologists (who finally diagnosed me); I finally expressed it to my therapist, whose cognitive behavior therapy is a recommended, helpful part of fibro treatment.
Related on The Swaddle:
What Sexual Dysfunction Looks Like When Female Sexual Dissatisfaction Is the Norm
What took me so long to get to that point? Well, centuries of the patriarchy shushing women who’d speak about their sexuality, and rapidly banishing their diatribes to the darkest recesses (while coming on their faces), is probably a good answer. That, coupled with the fact that women’s pain is also as undervalued, if not more, makes for a potent combination of familial ignorance, medical indifference, and sexual misogyny. Women, at whatever age they start to think of themselves sexually, are taught to stop. Immediately. They’re taught to inhibit their desires in bed, in marriages, in partnerships. They’re taught to be okay with giving oral sex but not asking for it. They’re taught that masturbation is taboo for them but a boy’s strong suit. Growing up, I can’t remember too many girls who spoke about whether they came during sex. How could I expect to find answers, then, on online chat groups and WhatsApp support forums from women with chronic pain, when they’d already been sexually inhibited for decades?
A study conducted on the sexual experiences of male partners of women with FM spoke about how men had realized they were “facing a new sex life” and were “resisting the loss of the couple’s sexuality” though.
That one hits home.
Feeling out a way forward
The jury’s out on what could definitively work, but the suggestions are simple: try oral sex, one Redditor says. Stimulate yourself first, another elucidates. Perhaps talk to your partner about what you’d like to try in bed? Move around the timings of your antidepressant dosages so you can make time for “sexy time” at your sexual peaks, a fourth expert claimed. My fifth internet guru gently nudged me into explaining to my partner that it “wasn’t about him or the relationship or the sex that we have”; it’s about the FM.
All sage advice, and all advice that I will be trying. But, here’s the thing. The problem doesn’t end with me having a conversation with an already incredible partner about why we are or aren’t having sex. The problem doesn’t end with a hundred more women with chronic pain syndromes and little-to-low arousal in their genitals having that conversation, either. We need a couple hundred, possibly millions more joining in – in the labyrinthine corridors of medical practitioners’ offices, in therapists’ chambers, and in family WhatsApp groups, where every part of the anatomy but the sexual is dissected to dust – to ask, listen, and empathize.
Only thing – when we do have those conversations, let’s forgo the whispers? Those dulcet decibels haven’t done much for women’s orgasms anyway.
Urmi Bhattacheryya is an independent journalist (formerly at The Quint), a feminist and chronic pain warrior, a trashy-reality-TV watcher (like you wouldn't believe) and a reader of reads.
Related


For People With Mental Health Conditions, Constant Covid19 Updates Make Everything Worse
