
Gender‑Affirmative Surgeries Are Helping Scientists Study the Clitoris Better
Scientists have counted 10,000 nerve fibers in the clitoris, revealing how gender-affirmative care can bridge knowledge gaps in sexual health.
In a first, scientists have counted more than 10,000 nerve fibers in the human clitoris, revealing how this part of the vulva — responsible for the experience of sexual pleasure — is much more sensitive than previously known. The clitoris has remained an under-studied part of human anatomy. Now, scientists say gender-affirmative surgeries and a focus on transgender health care is making it possible to study it in greater detail — research that has implications for sexual health.
Known as the only human organ whose sole purpose is to produce pleasure, the clitoris was previously believed to have 8,000 nerve fibers. The origins of this number, however, are contested. This popular statistic came from research on livestock, where a study on cow clitorises was extended to human beings. While the tip of the clitoris, the highly-sensitive clitoral glans, is found outside the body, most of the clitoris is located internally. The clitoral nerves control blood flow and are responsible for relaying information about pain, pleasure and touch.
There’s been a historical sexist bias in medical research that has led to the clitoris being sidelined. “It’s completely ignored by pretty much everyone… There is no medical community that has taken ownership in the research, in the management, in the diagnosis of vulva-related conditions,” Dr. Rachel Rubin, a urologist and sexual health specialist told The New York Times. But its role in gender-affirmative health care is being increasingly recognized — leading to more research about the organ as one that’s integral to sexual and reproductive health.
“Better understanding the clitoris can help everyone, regardless of their gender identity, but it’s important to acknowledge this research is only possible because of gender-affirming surgeries and transgender patients,” said Dr. Blair Peters, who led the latest study at the Oregon Health & Science University. The team’s findings were presented at a joint scientific meeting of the Sexual Medicine Society of North America and the International Society for Sexual Medicine. Their paper is currently being peer-reviewed at a scientific journal.
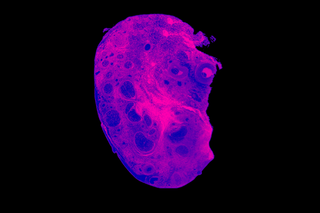
Peters’ team voluntarily obtained clitoral nerve tissue from seven transmasculine patients who had undergone gender-affirming genital surgery. The tissues were dyed blue and magnified 1,000 times so image analysis software could count the individual nerve fibers. While the counting revealed over 10,000 nerve fibers in dorsal nerve tissue, Peters stated that the clitoris also has many smaller nerves, making the grand total much higher.
Related on The Swaddle:
In a First, Scientists Find the Brain Region Linked to the Clitoris
While the penis has been extensively studied, significant knowledge gaps exist in the case of the vulva, and in turn, the clitoris. Its association with female pleasure and orgasms — topics that continue to be considered taboo — has resulted in its dismissal by the medical fraternity. This, however, has several consequences for sexual health. A report in The New York Times noted that the clitoris can be easily damaged during hip surgeries, pelvic mesh surgeries or episiotomies that involve making a cut to increase the opening of the vagina during childbirth. In a 2018 paper, researchers pointed out that physical examinations of the vulva and clitoris should be regularly carried out. However, the medical curriculum has long ignored this organ too.
Gender affirmative healthcare could be changing this paradigm. “Understanding the full shape of the clitoris… helps surgeons to spare crucial nerves during pelvic surgery, improve gender-affirmation procedures and repair the clitorises of women who have undergone female genital mutilation,” Scientific American noted. It can also help select and connect nerves during phalloplasty surgeries — a procedure that creates a new penis for transmasculine individuals using tissues from other parts of the body — for improved sensation. Some transmasculine individuals who undergo phalloplasty report diminished sensitivity in their neophallus — showing how understanding the clitoris is key.
Related on The Swaddle:
An Anatomical Guide to Female Genitalia for Anyone Who Needs It
It can also be applied to develop new techniques to repair injured nerves. For patients who undergo labiaplasty — a cosmetic surgery that reduces the size of the vaginal opening’s inner flaps — a greater understanding of clitoral nerves can help reduce accidental nerve damage that could lead to pain and a loss of sexual stimulation.
Research further underscores a need to unravel how gender-affirming surgeries and hormone therapy impact genital functioning and sexual health, which could inevitably lead to more studies on the anatomy and functioning of genital organs such as the clitoris. A paper published last year stated that gender-affirming medical care on the vaginas of transmasculine and transfeminine individuals is “poorly characterized,” with implications for gynecological health and treatment.
There are negative consequences to not understanding the clitoris properly. One case study highlighted how a transgender male who underwent gender-affirmative surgery developed painful and persistent clitoral engorgement — signs of clitoral priapism, which is a rare condition requiring urgent care. The authors suggested testosterone-induced anatomic changes of the clitoris “may adversely affect venous outflow,” outlining a need for further research into whether hormone therapy is a risk factor for priapism in transgender males. Other research points out how hormonal therapy could lead to clitoral pain in some trans men — which impacts their sexual health.
Gender-affirmative health care, then, has the potential to create opportunities to bring sexual health into mainstream discourse, improving health outcomes for all. In the future, Peters hopes to count nerve fibers concentrated at the tip of the penis too, which could inform clitoral construction in transfeminine patients. “There’s something profound about the fact that gender-affirming care becoming more commonplace also benefits other areas of health care. A rising tide lifts all boats. Oppressing or limiting transgender health care will harm everyone,” Peters said.
Ananya Singh is a Senior Staff Writer at TheSwaddle. She has previously worked as a journalist, researcher and copy editor. Her work explores the intersection of environment, gender and health, with a focus on social and climate justice.
Related


‘Smart’ Red Blood Cells Could Address The Antibiotic Resistance Crisis, Scientists Say
