Globally, a Lack of Awareness Is to Blame for Ovarian Cancer Fatalities
Doctors and patients alike don’t know enough about gynecological cancers.
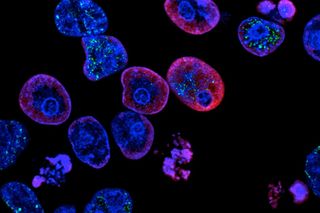
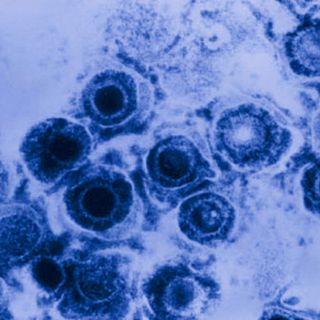
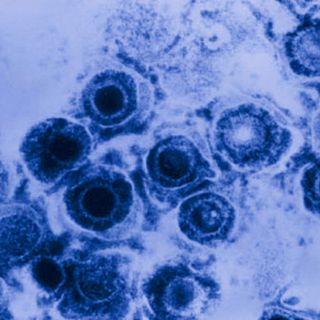
Around the world, women suffer most from four types of cancers: breast cancer, cervical cancer, ovarian cancer and uterine cancer, also known as endometrial cancer. And in India, they account for more than 70% of the cancers in women — yet most women remain unaware of their prevalence, or even of the diseases themselves. The lack of awareness decreases women’s chances of survival. This is especially true for ovarian cancer.
“… Most patients of ovarian cancer come with advanced disease because there are no screening tests or definitive early symptoms of ovarian cancer,” Dr Yogesh Kulkarini, a gynecological oncology surgeon at Mumbai’s Kokilaben Dhirubhai Ambani Hospital, told Livemint. Other cancers are easier to diagnose.
A recent global study seems to corroborate his observations. After surveying more than 1,500 women, in more than 44 countries, researchers found that two-thirds had never heard of ovarian cancer, or did not know anything other than its name, before their diagnosis. Nine out of 10 had experienced symptoms prior to diagnosis, but fewer than half of those women visited a doctor within a month of noticing symptoms.
This sheds some light on ovarian cancer’s grim statistics; of the approximately 239,000 women who are diagnosed with ovarian cancer each year, less than half of them survive to five years. Around 15% of women die within two months of their diagnosis; age, emergency presentation, and the presence of one or more diseases placed them at increased risk, the study revealed.
And by 2035, the incidence of ovarian cancer will rise by 55% simply because people are living longer and there have been far fewer breakthroughs in the disease’s diagnosis and treatment, said the study.
According to a survey participant in Australia, “Governments need to do more regarding [family doctors] and their lack of diagnosis and interest in women with ovarian cancer. After diagnosis, I Googled, and all my symptoms were mentioned. GPs were not interested enough and made me feel like a hypochondriac. This went on for months!”
The study, too, said that the patients’ lack of understanding wasn’t the only problem, “Lack of awareness among doctors may also be a significant factor when it comes to delays in diagnosis.”
Across the world, including India, diagnosis took an estimated average of 31 weeks from a woman experiencing symptoms to her diagnosis; for one in ten women, diagnosis came more than a year after visiting a doctor.
There are examples of best practices in prevention, diagnosis and treatment of ovarian cancer across the world, but no one country does well in all three areas. “This means there are opportunities right now to transform survival in ovarian cancer, simply by learning from what others do well,” reported the study.
Germany, for example has the fastest diagnosis, yet it is estimated that half of women are unlikely to receive specialist care. The UK, by comparison, has the lowest proportion of women diagnosed within a month of visiting a doctor, yet almost universal access to specialist clinicians. Similarly, Australian women had a longer time to diagnosis — but high rates of successful surgery.
India’s problems include all of the above. In addition, acceptance is a big stumbling block; denial is often one of the major factors that delays women getting timely diagnosis and treatment. The shame women’s reproductive cancers evoke means even the women who notice symptoms often hide their worst suspicions.
Many of these issues are endemic to women’s health overall, but doctors say examining them in the context of ovarian cancer is a helpful start to providing better care — and improving survival rates.
“We are pleased to have completed this study, which gives us an idea of the changes that can be made to help women with ovarian cancer,” says Dr Neerja Bhatla, who chairs the gynecologic oncology committee of the International Federation of Gynecology and Obstetrics and who was the clinical co-chair of the study. “We need to build support and funds for action to achieve profound and long-lasting change for women with ovarian cancer.”
Anubhuti Matta is an associate editor with The Swaddle. When not at work, she's busy pursuing kathak, reading books on and by women in the Middle East or making dresses out of Indian prints.
Related

How Much Protein Do You Really Need?
