Infertility in Men: Here’s How Sperm Can Be Compromised
Sperm quality is affected by a variety variety of physiological, environmental and lifestyle factors.
27.5 million couples in India struggle withinfertility, reveals data from a Bengaluru-based medical technology company. And while infertility — defined as the inability to conceive following 12 months of regular sexual intercourse without the use of contraception — is commonly perceived as a woman’s problem, we all know it takes two to conceive and make a baby. The latest report on the status of infertility in India, by the World Health Organization, stated that out of all infertility cases, 50% are caused due to ‘male factors.’
The most significant factors among men that contribute to difficulty in conceiving include: low sperm count, poor sperm movement, abnormal sperm shape, and poor sperm quality. Here’s all you need to know about the four most common fertility issues for men:
Low sperm count
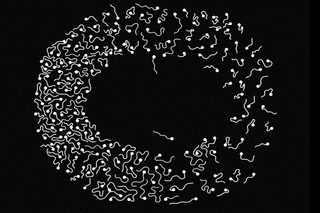
Low sperm count, technically known as oligospermia, means that the semen a man ejaculates during an orgasm contains fewer sperm cells than the common average. A man’s sperm count is considered lower than normal if he has fewer than 15 million sperm per milliliter of semen. Having a low sperm count can decrease the chances of conceiving a child simply because it means fewer opportunities for fertilization. Low sperm count is caused by a variety of physiological, environmental and lifestyle factors, from infections, hormonal imbalances, and autoimmune problems, to emotional stress, depression and obesity.
One of the most common physiological causes, varicocele, is responsible for 40% of cases of low sperm count. A varicocele is a group of dilated veins in the scrotom. For most men they don’t cause any problem. For some, however, the dilated vessels increase the temperature of the scrotum, resulting in pain, testicular damage and impaired sperm production. Many men with varicocele are able to conceive without problems, but those who experience pain or infertility might want to undergo a surgery to repair the veins. The repair surgery seals off the dilated vein and redirects the blood flow into normal veins. This may cure the infertility (i.e. normal sperm production resumes) and/or improve the quality of spermallowing for in vitro fertilization (IVF), if not natural conception.
Poor sperm movement
Sperm motility is the ability of sperm to move efficiently. It is important in fertility because sperm need to move rapidly and directly through the woman’s reproductive tract in order to reach and fertilize her egg before the sperm cells die.
Dr. Aditi Dani, a fertility expert at Mumbai’s Masina Hospital, explains there are two kinds of sperm motility: progressive motility and non-progressive motility. Progressive motility refers to sperm that are swimming in a straight line, and non-progressive motility refers to sperm that do not travel in straight lines. For the sperm to fertilize a woman’s egg, they need to have progressive motility of at least 25 micrometers a second. Poor sperm motility is diagnosed when less than 32% of the sperm in a semen sample are able to move at that speed or are not traveling in straight lines.
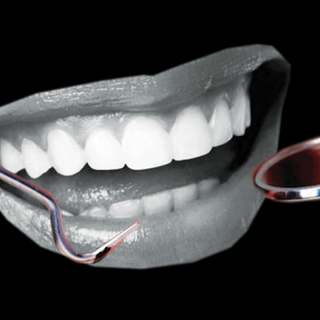
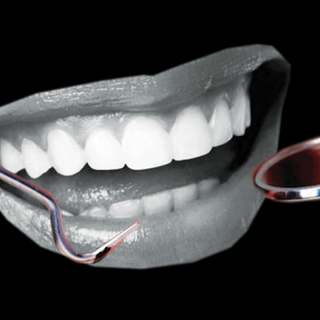
Damage to the testicles, which make and store sperm, could be a reason to low sperm motility. Semen analysis is the most basic and useful test to diagnose poor sperm motility, as well as other fertility problems.
Poor lifestyle choices contribute to sperm issues; some of those factors are age, alcohol and tobacco consumption, and obesity.
Abnormal sperm shape
Sperm morphology refers to the size and shape of sperm, and is another factor that’s tested as part of a semen analysis check. Normal sperm have an oval head with a long tail. Abnormal sperm (teratospermia) have faulty heads, or tail anomalies. These faults might affect the ability of the sperm to reach and penetrate an egg.
To assess sperm morphology, the sperm from a semen sample are examined under a microscope. Almost all men naturally produce some abnormally shaped sperm; as many as half of the sperm in a “normal” semen sample appear unusual.
What causes some men to produce more unusually shaped sperm than others isn’t clear; research has not shown a relationship between abnormal sperm shape and tobacco, alcohol, or caffeine use, though some studies suggest that smoking can contribute to abnormal sperm shape. Men with abnormally shaped sperm tend to have more trouble conceiving, but it cannot be said for sure whether that difficulty is caused by the shape of the sperm or by another reason that causes the sperm to be shaped differently and at the same time causes a problem with fertility. That said, the shape of sperm is typically a factor in whether a couple is advised to pursue IVF.
Sperm quality
Another factor affecting male infertility is sperm quality — that is, fragmentation of the DNA contained in a sperm cell. Degradation of sperm DNA affects the health of an embryo’s genetic make-up, and can contribute to miscarriage.
After men turn 40, the quality of their sperm’s genetic material lessens; even as their bodies continue to constantly produce new sperm, the new sperm isn’t as good as the sperm they produced when younger. It’s a natural and irreversible effect of aging, much like how women’s eggs deteriorate after age 35. This disguises a major factor in fertility struggles, like repeat miscarriage: declining sperm quality may not impact men’s ability to ejaculate or successfully fertilize an egg, but it is more likely to make an embryo unviable.
Miscarriage is the body’s way of dealing with a pregnancy that can’t proceed further due to genetic abnormalities. Since miscarriage occurs only in women, it is often assumed, or secretly felt, that when it does, there is something wrong with the mother. Yet, it’s just as likely the male contribution is responsible; when one half of the genetic material is degraded from the start — as in the case of men over 40 — it makes it more difficult for an egg to fertilize in a way that’s viable. The result is often an embryo that’s not chromosomally sound enough to develop into a fetus and baby — thus, miscarriage.
So while a man over 40 may be highly fertile on paper (that is, he may not experience difficulty ejaculating or a low sperm count), his age — not just his partner’s — may still be a factor in fertility problems.
According to experts, if that happens, couples are often advised to make better choices about the right lifestyle and the best fertility treatment for them. For instance, IVF could be the best treatment to try if there’s moderate damage. IVF can allow couples to select a healthy sperm; ‘natural’ conception is basically a roll of the dice whether you get a sperm with high-quality DNA, or not.
Avoiding known factors such as smoking, abstaining from drinking, exercising, managing stress and keeping away from heavy metals, pesticides and other toxins could help in maintaining healthy sperm quality.
Sanskrita Bharadwaj is a freelance journalist. Some of her bylines have also appeared in Scroll, the Hindu, Indian Express, IndiaSpend, Quint, Firstpost, and The Wire. She has previously worked at the independent publishing house, Aleph Book Company in New Delhi as an assistant editor.
Related

Untrending: The Keto Diet Might Help Weight Loss, But That Doesn’t Make It Healthy