Doctor Diary, Day 4: “I Have Five Days of Quarantine Ahead of Me. I’m Dreading It.”
“I’ve made up my mind — I’m not going to obsess. I’m going to unwind and not think about the last few weeks of my life,” she says.
A 28-year-old anesthetist working in the Covid19 I.C.U ward of a private Mumbai hospital, currently run by the BMC, shares the ups and downs of her days on the frontlines fighting the Covid19 pandemic. This is the fourth installment of a daily diary she shares with The Swaddle.
Doctor Diary, Day 3: “I Do Miss Human Contact…I Can’t Even Hug Someone.”
*
Afternoon: Doing administrative work It was madness today. The minute I went in, I learned that two patients had passed away. A third one had just died when I got in. I didn’t even know these patients; they had been admitted yesterday. I asked the medicine lecturer to help me out — he knew a little bit about the patients. I helped him finish the death formalities.
When you fill the form, you have to get exact details from the relatives, in the middle of declaring the patient dead. You have to ask them for the address, age — all basic things from their Aadhaar card. It’s a legal document so everything needs to be perfect. It seems very mean to do this, but you hope they understand. You try to make it less inhumane.
We were short of people today. The juniors who trace labs — they weren’t in. In the afternoon, a lot of labs came in so I had to enter them, change my medicine orders accordingly. We also used five new ventilators today, so I checked them all, shifted them inside the I.C.U. Then I got a call that a couple of patients weren’t doing well, but I had to wait outside for a while before I went in, as leaving the phones unmanned is not an option. We can’t miss any calls asking for patients needing to get admitted.
It’s my last day at this hospital today.
Evening: Doing rounds When I went to collect my scrubs, I met my associate professors in charge of the I.C.U. They wished me all the best, said it was nice working with me. It feels good that I’ve helped them in some way, that they consider me to have been significant enough.
Today, there’s yet another PPE. It was even worse — we had to tape a lot of it to pull it together. Not that we couldn’t make do — I’m just used to better. Maybe it’s because the people who donate the PPE to us keep changing — they’re donors so they probably don’t know what works and what doesn’t.
In the beginning, we used to get so worried about even a single inch of skin being exposed to the environment. But we figured out that it’s not as bad as we think it is. Most of the time, the only exposed part is your cheek, and even there, we have some shade. Although at the end of six hours, most of us are just waiting for someone to come, so we can leave and get out of the PPE.
Today, as soon as I went into the I.C.U., they told me a young 35-year-old woman was coming in. She was doing really badly, was already on the ventilator. Luckily, she’s holding on, but I don’t know where this is going to go.
The other patients are also not doing so well — they will possibly require intubation. Judging from my past experience, however, I’m deciding to let them hold on as long as they can before I put them on ventilators. This also takes a mental component — you have to console them because otherwise, they get really agitated. You have to calm them down. They were showing some improvements so I decided not to intubate.
I can see the change — it’s drastic. Over the last week, the number of calls we get for beds has increased, and the patient turnover is huge. Now, with the I.C.U. full every day, we have to shift the slightly better patients to a step down I.C.U., to give the remaining ones a fighting chance.
I stayed until 8:30. It’s my last day, so there’s no point in running. I had nothing to lose.
Nightfall: Saying goodbyes I spoke to the nursing staff on my way out. I have become very friendly with them. I wished them well. I don’t even know half of their names, but we’ve always sat and chatted over chai. We’ve formed a bond. We have a group chat where we discuss patients. I have everyone’s numbers, so I’m going to keep in touch.
I’ll miss the socializing at work a lot. I have made so many friends — from residents to nurses. I also hate being cooped up in one place. At work, there’s definitely an adrenaline rush. Whatever the outcome, there’s this rush that comes with doing something useful. Anesthesia is usually described as moments of terror and hours of boredom. Right now, it’s all terror but it keeps you going. That’s what we live for. After so many years of training, you start obsessing about what you do.
I’m already feeling a tinge of regret, sadness, that I couldn’t learn as much as I wanted to. I couldn’t do as much as I wanted to. In the hospital I’m leaving for, the I.C.U. is under the anesthesia department, so you learn mostly about breathing-related issues. Here, it’s under general medicine. These doctors know more about I.C.U. management, so there was a lot to learn — nutrition, even some surgical aspects. That’s what helps patients get better. Here, they also have negative pressure I.C.U.s — it’s like a vacuum that is created, to control air pressure that prevents cross-infection among patients, and also infection to us. The air conditioning is off, and then we have negative pressure in its place. Where I’m going, they don’t have that. They’re also dealing with equipment shortage.
I’m less sad about leaving here and warier of getting back to a place where things are not as good as they are here. Things are going to get worse and it’s going to take a much worse toll on my emotional well-being. It’s going to be harder. That’s what scares me more than leaving — the fear of the unknown is what’s killing me. But once I get there, I’ll figure it out.
Night: Gearing up for quarantine I couldn’t stomach my dinner today. I just had some milk and bournvita. So many things happened today — because it all happened so fast, I couldn’t think about the death as much as I normally do. You have to think about it mechanically. But then when you sit back, you’re sucked in. Now, I have five days of quarantine ahead of me — I’m dreading it because I’ll have time to mull over things.
I didn’t know the patients who died today. I hadn’t formed a bond with them. When I’m told a patient has died whom I didn’t know, it doesn’t kill me as much as when I’ve known them for a week and seen them crashing. But I don’t like it being this way.
The first thing I’m doing is muting the I.C.U. group — the more I see, the more I get affected by it. It doesn’t look good, I know, but my emotional wellbeing is more important. My colleagues will still come back from work and tell me things, so it’s not like I’m going to be completely free.
I’m going to try and zone out as much as possible. I’m not going to look at statistics, hospital data. I have five days to do nothing. I’ve made up my mind — I’m not going to obsess. I’m going to unwind and not think about the last few weeks of my life.
I don’t have any company. I don’t have a choice so I’m going to be my own company. I’m learning how to crochet, so maybe I can make some small thing. I’m still learning so it’s going to take up a lot of my time. I’m also going to binge watch a lot of things — just today, I was told to watch Younger, which is supposed to be a light, easy watch. I also have my kindle — Sapiens has been on my list forever. I also have some Agatha Christie on there.
And I’m going to obsess about cleaning my room a thousand times.
I was playing around with the idea of just taking a throat swab and going back home. But I’m worried — if it turns out positive, it’s much worse. You have to undergo the whole rigamarole of getting the procedure done, be stuck in a room, plus there’s the whole stigma of being Covid19-positive. I’m dreading that — I’d rather not test until I fall sick.
As told to Rajvi Desai.
Doctor Diary, Day 5: “It’s the First Day of Quarantine. I Kept My Promise of Minimal Covid19 Talk.”
Related
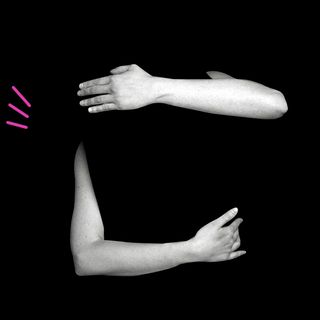
We’re All Touch‑Deprived Under Lockdown. It Can Affect Our Self‑Perception.