
Study: Awareness, Availability of HPV Vaccine Does Not Increase Risky Sexual Behavior in Teens
But it does require us to recognize kids as future sexual beings.
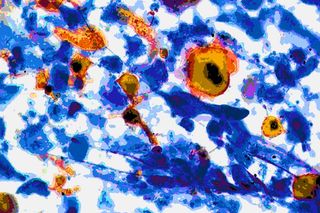
One of the arguments against administering the HPV vaccine to teens is that by preventing a possible human papillomavirus infection — which can later develop into cancer — it will encourage them to indulge in riskier sexual behavior. It’s the same argument wielded against sex education: teaching kids about sex will only make them have more of it, and sooner.
Except, just as studies have proven that argument against sex education false, now a large-scale study, published by the American Academy of Pediatrics, is proving that argument against the HPV vaccine false, too.
The researchers analysed data from more than 800,000 high schoolers across 41 US states — 25 of which do not have any HPV-related legislation, and 16 of which do have some kind of law around HPV vaccine cost, availability and/or education — collected via annual national youth health surveys. The data spanned 2001 to 2015, several years before and after most HPV-related laws were enacted.
The team focused on three main questions: If students had had sex at any point in the previous three months; if students had used a condom during their last sexual encounter; and how many sexual partners students had had in the previous three months. They then compared results, controlling for age, race, sex and class level, from before and after HPV-related laws came into effect, and between states that had HPV laws on the books, and states that did not.
They found no statistically significant difference in teen sexual activity or proclivity for unsafe sex in any comparison — before and after legislation, or between states with different legal requirements. If anything, students in states with HPV-related laws — and therefore improved access to and awareness about the vaccine — reported slightly less recent sex and slightly safer sex; but since the differences were less than 1%, the findings are negligible.
In other words, making the HPV vaccine affordable and available, and making teens aware of its benefits, does not lead them to have more sex.
Related on The Swaddle:
Which means there’s nothing standing in the way of virtually eliminating HPV infection — and with it, most cases of cervical cancer in women, and some cancers in men — but our own inability to think of children as future sexual beings. In a culture where sex, even consensual sex between adults, is taboo and sometimes illegal, that’s a difficult hurdle to cross. The ‘morality’ hang-up may be what has led some eminent doctors to argue — mistakenly — that HPV screenings can accomplish the same thing as a vaccine. They can’t; but for many people, it’s more acceptable to examine an adult’s genitalia and maybe catch a preventable disease before it turns deadly, than to acknowledge that a child will one day be one such sexually active adult (or may already be a sexually active adolescent), and take preventative measures.
In the end, there is no good reason not to institute the HPV vaccine as a standard vaccination for both girls and boys. Its safety and effectiveness in reducing cervical cancer rates has been proven time and again. And now, there’s no evidence it makes teens more sexually active, or riskier in their sexual activities. So, what are we waiting for?
Liesl Goecker is The Swaddle's managing editor.
Related


‘I Scheduled My Own C‑Section,’ She Said, ‘Because I Had a Job Interview’
