
Survey Shows Most Indians Are Confused About Contraception. Are You One of Them?
So, let’s clear up some things.
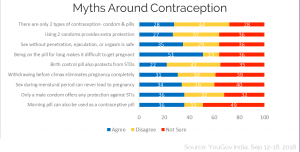
A recent online survey of 1,000 Indians revealed that the country is rather confused about contraceptive methods — what birth control options are available, what are most effective, and how they work. Per YouGov, the market research firm behind the poll:
So if these are myths, what are the facts? Let’s break it down.
3 in 4 Indians surveyed believe there are only two types of contraception — condoms and pills — or aren’t sure if there are more.
In fact, there are many different birth control options. Women have a broader set of options — some of which are as or more effective than condoms and pills. Men, currently, only have one: condoms.
The same number believe using two condoms at the same time is more effective than using one only, or they aren’t sure.
In fact, using two condoms is not more effective than using one condom — and may be less effective: The friction of the two condoms rubbing against each other can weaken the material and cause the condoms to break.
65% of Indians surveyed believe sex without penetration, ejaculation, or orgasm is safe, or they aren’t sure.
First, even if men don’t ejaculate/orgasm, they still release a substance called pre-ejaculate, which can carry sexually transmitted infections like HIV. Pre-ejaculate can also pick up sperm from previous ejaculations as it passes through the same tube as semen. Which means this pre-ejaculate can contain a few sperm, posing an low, but possible chance of pregnancy.
Second, even without penetration, ejaculation or orgasm, STIs can be passed between people via skin-to-skin contact and oral sex.
Half of people surveyed believe being on the Pill for ‘too long’ makes it difficult for women to get pregnant, or they aren’t sure.
While women might experience other possible side effects of using hormonal contraceptive pills regularly and for an extended period of time (we’re talking years), there is no concrete evidence that lengthy use of birth control pills damages inhibits fertility. There is, however, a related misconception that might be driving this myth: That the birth control pill ‘cures’ irregular menstrual cycles. It doesn’t; instead, it regulates the menstrual cycle, but as soon as a woman goes off the pill, its effects stop. Meaning, if a woman had an irregular menstrual cycle (irregular ovulation) before going on the pill, she’ll have that same issue after going off the pill — and this underlying irregularity may make getting pregnant more difficult.
An overwhelming 4 in 5 people surveyed believe birth control pills can protect against STIs, or they aren’t sure.
Most birth control pills work by regulating a woman’s hormones to levels that prevent ovulation — thus preventing her from being able to become pregnant. They have absolutely zero effect or relationship to STIs.
70% of people surveyed believe withdrawing before climax means there is zero chance a woman can become pregnant, or they aren’t sure.
While withdrawing before climax certainly reduces a woman’s chance of becoming pregnant, it is not the foolproof contraceptive method that many appear to think. Because pre-ejaculate can contain sperm, it’s entirely possible for a woman to become pregnant, even if a man does not ejaculate inside her.
2 in 3 Indians surveyed believe women can’t get pregnant from period sex, or they aren’t sure.
While a woman’s odds of getting pregnant on day 1 or 2 of her period are close to nil, the likelihood rises each day after that, even if she’s still bleeding. Women with shorter cycles have greater likelihood (even if it’s still low) of getting pregnant from sex while they’re still bleeding. Finally, some women also bleed during ovulation — when they’re at peak fertility — which they might mistake for their period, particularly if they have irregular cycles.
The same number think male condoms are the only method of protection against STIs, or they’re not sure.
In fact, female condoms can also protect against STIs. Both are the best, most effective methods availble for STI protection, even if neither is foolproof against infection.
And the same number think the morning-after pill (aka, the iPill) can also be used as regular contraception, or they’re not sure.
Technically, emergency contraception can be used regularly. The problem with doing so, however, is that the morning after pill is much less effective than most other contraceptive methods; studies put its effectiveness at preventing pregnancy at 52-100% — compared to condoms, which are solidly 98% effective, the pill (99% effective), and IUDs, which prevent pregnancy more than 99% of the time.
The morning after pill can also cause side effects like nausea, vomiting, irregular bleeding, and depression, which can be unpleasant if experienced on a regular basis — but reports of more serious health effects of taking the morning after pill ‘too much’ are overblown.
Liesl Goecker is The Swaddle's managing editor.
Related


Can Stress Affect Fertility? Study of 5,000 Women Says Probably.
