Study: Untreated Brain Injury Common in Survivors of Domestic Violence
Repeated head injuries and oxygen deprivation could cause a slew of physical, mental and cognitive problems.
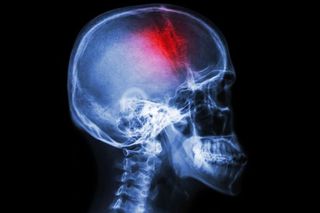
People who have survived violence at the hands of a current or ex-intimate partner might be walking around with undetected brain injuries, according to a new community-based study published in the Journal of Aggression, Maltreatment, and Trauma. The study states survivors who have experienced repeated head injuries and oxygen deprivation can suffer memory loss, poor cognition, loss of motivation, nightmares, anxiety, and trouble with hearing and vision from internal injuries.
“These women could be having trouble being able to plan for the future, to make decisions about their safety, to come to appointments, to do their jobs. Many have likely been wondering for years what’s going on with them,” Rachel Ramirez, co-author of the community-based study and a training director for the Ohio Domestic Violence Network, said in a statement.
Previous research has linked intimate partner violence to traumatic brain injury, and another major study published in 2019 found via neuroimaging that abused women had less interaction between two areas of the brain important to everyday function. The less the interaction between these regions, the worse these people performed on tasks associated with memory and learning.
By definition, a concussion is a traumatic brain injury. These injuries are often missed, however, because people who experience intimate partner violence might hesitate to seek help due to societal stigma against domestic violence, or due to manipulation by their abuser. Often, survivors of such violence return to their partners, which could cause further abuse and compound any damage caused by previous injuries. Beyond traumatic brain injury, survivors may also experience PTSD, depression and anxiety.
A lack of awareness around the risks of brain injury among support systems for survivors is also part of the problem, experts say. Most medical research and recommendations for treating traumatic brain injuries are focused on athletes and soldiers, who are professionally susceptible to concussions. The hyper-focus on those two groups means there’s barely any awareness about the concussion risk for domestic violence survivors. This means common refuges for survivors of intimate partner violence, like women’s shelters and NGOs, are not well equipped to anticipate or detect traumatic brain injuries among the population they help.
“The fact is, the staff at women’s shelters and many other women-serving agencies generally don’t have the knowledge, training or tools to screen for brain injury at intake. This means many [intimate partner violence] survivors who have suffered a traumatic brain injury are not getting the support they really need to accomplish their goals and move forward into a life free of abuse,” wrote the researcher and University of British Columbia professor Paul van Donkelaarin in The Conversation.
Related on The Swaddle:
‘Why Didn’t They Leave?’ and the Vicious Cycle of Abusive Relationships
Dr. Eve Valera, an assistant professor in psychiatry at Harvard Medical School, writes in the Harvard Health Blog that the only thing required for someone to sustain a traumatic brain injury or concussion is an alteration in consciousness after some type of external trauma to the head. “For example, either being hit in the head with a hard object (such as a fist) or having a head hit against a hard object (such as a wall or floor), can cause a traumatic brain injury,” she writes. “If this force results in confusion, memory loss around the event, or loss of consciousness, this is a serious injury. Dizziness or seeing stars or spots following such a force can also indicate a traumatic brain injury. A loss of consciousness is not required, and in fact, does not occur in the majority of mild traumatic brain injuries.”
Valera also added that post-concussive symptoms span a range of physical, emotional, behavioral and cognitive issues and include headaches, dizziness, feeling depressed or tearful, being irritable or easily angered, frustration, restlessness, having poor concentration, sleep disturbances, forgetfulness and taking longer to think.
30% of women around the world have suffered intimate partner violence, according to a World Health Organization report. In the WHO African, Eastern Mediterranean and South-East Asia (which includes India) regions, this number jumps to 37%. The exposure to violence, peaking at ages 40-44, begins for women as young as 15-19.
Aditi Murti is a culture writer at The Swaddle. Previously, she worked as a freelance journalist focused on gender and cities. Find her on social media @aditimurti.
Related


Could Intuitive Eating End Diet Culture?