Undiagnosed Sexually Transmitted Infections Can Make PMS Worse
Many STIs don’t have noticeable symptoms. Get tested.
A new study has found that having an STI, that is, a sexually transmitted infection, can affect your period by worsening premenstrual syndrome symptoms. And if you’re thinking, “Oh, that’s fine, I don’t have an STI” — think again. Many sexually transmitted infections don’t manifest obvious symptoms in women, which means they go undiagnosed, making PMS more severe, like invisible hype men at a particularly misogynistic rap concert.
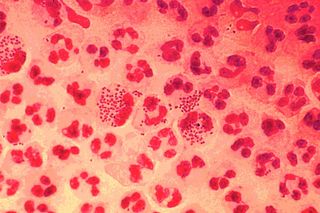
More specifically, researchers found that prior to diagnosis, the presence of an infection such as chlamydia, herpes or HPV doubled the likelihood a woman would report PMS symptoms such as general sensitivity, headaches, cramps and sadness.
These infections are all typically asymptomatic, and more common than you might think. In India, private labs reported last year a 20% increase in cases of HPV and herpes. While this is likely due in large part to better access and screening, it is part of a broader trend; many STIs, especially those that are treatable like chlamydia and gonorrhea, are making a global comeback through antibiotic resistance.
“Not understanding or even acknowledging that PMS is more than ‘women’s raging hormones’ … makes it harder to identify diseases and can even delay diagnosis of infections, such as STIs, which can affect women’s fertility,” says the study’s lead author Alexandra Alvergne, PhD, an associate professor of anthropology at the University of Oxford, UK.
Alvergne and team analysed data on menstruation patterns, contraceptive use, pain and emotional health from more than 800 users of the period-tracking app CLUE. The users also completed questionnaires regarding their history of STIs, including date of diagnosis and treatment.
“Our research shows that by better understanding their period and menstrual cycle, women could potentially improve their health. If you know that severe PMS could be an indicator of an underlying STI, you are more likely to listen to your body,” Alvergne says.
The problem is, she adds, the medical establishment doesn’t set much stock in this link between menstruation and immunity. Instead, the generally accepted view is that ‘raging hormones’ are the cause of PMS and menstruation is an isolated, if regular, aberration from normal health. But Alvergne says this study bolsters a growing, alternative narrative: that far from being an isolated event, the menstrual cycle is part of a broader cycle of immunity aimed at fostering viable embryos and regulating overall good health.
Alvergne makes the case for this view in the journal Evolution, Medicine & Public Health, citing other studies that have found the severity of chronic inflammatory diseases or the risk of infection depends on which phase of the menstrual cycle a woman is experiencing.
“The whole function of the menstrual cycle is to produce cyclical patterns of immunity, so actually we would be better to think of female health as cyclical. To truly understand women’s health we need to better understand reproductive health, as the two go hand in hand,” she says.
Liesl Goecker is The Swaddle's managing editor.
Related

Encouraging Kids Can Backfire If You Don’t Get the Wording Right
