
Study Links E‑Cigarettes to Immune Damage as Mystery Vaping Sickness Claims Seventh Victim
Sensing the frenzy in the West, the Indian Cabinet of Ministers has decided to ban the production, import, distribution, and sale of e-cigarettes.

Inhaling e-cigarette vapor, even without any nicotine, could fundamentally alter important cells that defend the lungs against infections, according to a recent study published in the Journal of Clinical Investigation.
With the goal to study how vaping alters lung function, researchers at Baylor University studied mice who were exposed to e-cigarette vapor and found their lungs’ defenses against bacteria and viruses were compromised, leaving their immune system out of balance.
This study comes at a crucial time, as a mysterious respiratory sickness related to vaping, sweeping the United States, is worsening: according to the U.S. Centers for Disease Control and Prevention (CDC), 380 people — mostly young adults — have been hospitalized across 36 states and seven have died; the Apple of the vape market, Juul, has been pulled up by the federal government for aggressively and falsely marketing e-cigarettes to young people; the CDC has activated its Emergency Operations Centre; and, President Donald Trump has sanctioned a temporary ban on flavored e-cigarettes that will be implemented in the next couple of months.
Sensing this frenzy, the Indian Cabinet of Ministers on Wednesday decided to ban the production, import, distribution, and sale of electronic cigarettes. This will now be floated as a bill, which if/when approved by the Parliament, will become the law regulating a vaping market valued at around $15.6 million presently.
But U.S. doctors still don’t know the root of the problem. They are still running test samples from products patients have used to find a common thread between cases, to figure out whether it is the type of e-cigarette, the brand or the substance being smoked that is causing this poorly understood illness.
However, some of the cases being investigated have been diagnosed as lipoid pneumonia, reports Wired, a condition that presents symptoms similar to pneumonia, but instead of being caused by a bacteria, it occurs as an immune response to fat build-up in the lungs. Researchers at Baylor found the mice developed a similar condition without ever inhaling nicotine or THC (a chemical compound found in marijuana) — substances that are usually smoked via an e-cigarette; “just the chronic exposure to the solvents [in the vape] was enough,” Farrah Kheradmand, a pulmonologist at Baylor who conducted the study, told Wired.
Related on The Swaddle:
Vape Liquid Can Negatively Impact Vascular Health, Even Without Nicotine
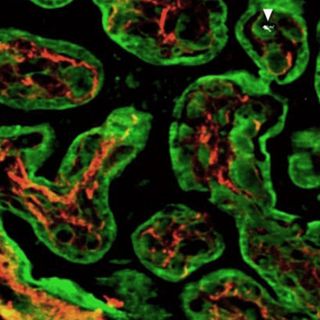
The primary function of the lungs is to regulate the exchange of gases. But since no air is perfectly clean air, the lungs have a mechanism to protect the body from pollutants, bacteria, and viruses in the air. They have a thin coating of lipids which binds all the toxins together, preventing them from reaching the air sacs. The lungs also have cells called macrophages, which destroy any toxins they encounter and also renew the lungs’ lipid lining several times a day.
Researchers found the solvents in the vape cartridges damaged the lipids in the mice’s lungs, and reduced the effectivity of the macrophages in recycling their lipid lining and screening out toxins. The solvents essentially changed the basic biology of mice lungs; when the researchers then exposed the mice to small amounts of the flu virus — amounts that would otherwise not severely affect a mouse — the vaping mice died, unable to fight off even a small infection.
Sure, mice are not humans and their lungs are different in size and cellular structure, but some of the initial research done on the effects of tar and tobacco was conducted on mice and later found to be applicable to humans as well. That being said, it is unlikely vaping solvents alone can explain this sudden outburst of the mystery illness. It could be toxic flavorings or poor quality THC laced with toxins compounded with nicotine, or vapes that burn chemicals at very high temperatures, or counterfeit vapes of poor quality — or a combination of any of these things.
To determine the cause of an outbreak of an illness, epidemiologists conduct what is called a case-control study in which they compare those with the illness (cases) to people similar to the cases but who didn’t get sick (the controls). In the case of this vaping illness, defining both components is turning out to be a significant challenge. People are presenting with a range of symptoms, for varying periods of time, so much so that doctors are yet to figure out if it’s one unknown syndrome or a handful of illnesses. It was only last month that the CDC set a barebones definition of a ‘case’: someone who has used a vape in the past three months, whose scans show spots on the lungs and no other signs of pulmonary infection or any other diagnoses. But, because the investigation into this vaping sickness hasn’t yet zeroed in on one suspect, health officials don’t know what control factors to choose. Should they compare sick patients to people who vaped but didn’t get sick? Or people who vaped THC to those who vaped nicotine in combination with THC? Or those who used an older vape to those who used more recent technology?
All we know for now, as the CDC is anxiously reiterating, is that vaping is no longer the benign alternative to tobacco smoking as it was initially marketed. Caution must be exercised because by the looks of it — vaping could kill.
Pallavi Prasad is The Swaddle's Features Editor. When she isn't fighting for gender justice and being righteous, you can find her dabbling in street and sports photography, reading philosophy, drowning in green tea, and procrastinating on doing the dishes.
Related

Study: Air Pollution Breathed by Pregnant Women Can Cross Placenta to Reach Fetus
