The Lowdown on the Very Common Condition of Uterine Fibroids
While uterine fibroids are not malignant, they can have serious, negative effects on one’s quality of life.
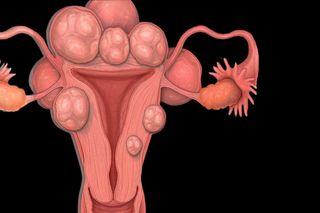
Uterine fibroids are dense, muscular, benign tumors that grow for no known reason in the wall of the uterus. They are not cancerous; they won’t become cancerous; and they don’t increase risk of uterine cancer. But uterine fibroids can significantly limit the lifestyles and comfort of people who have them.
This is not a small number of individuals. While the prevalence of uterine fibroids — officially known as leiomyomas, or myomas — is unknown, various expert sources suggest anywhere from 20% to 80% of all women will have at least one of these masses at some point in life, if not more.
In light of the potentially staggering number of people affected, uterine fibroids don’t feel like they’re discussed enough. (They certainly haven’t been researched enough.) So, let’s dive in.
What triggers uterine fibroids?
No one knows what triggers the initial growth of uterine fibroids. Experts suspect genes play a role, as fibroids tend to run in families. And they know hormones play a role, even if they’re not sure how. Fibroids grow under the effect of estrogen and progesterone, and shrink when the supply of those hormones ebbs — in response to hormone suppressant medication or menopause. In fact, uterine fibroids either stop growing or shrink once a person hits menopause.
Experts also believe fibroids are influenced by other substances that prompt tissue growth — such as insulin-like growth factor — as well as the extracellular matrix, the material that helps cells stick together to form tissue. Extracellular matrix stores growth substances, and is known to be thicker in fibroid tissue, according to the Mayo Clinic.
Nothing else — neither diet nor lifestyle — has been proven to prompt fibroid growth.
How big do uterine fibroids grow?
Uterine fibroids come in as many varieties as the people who have them — from “the size of a pea to the size of a watermelon,” according to UCLA Health. Fibroids also grow at different rates, even within the same person. It’s impossible to predict how big a fibroid will grow. However, the bigger the fibroid(s), the more likely a person is to experience symptoms that inhibit their quality of life.
Related on The Swaddle:
Why Women Are More Prone to Urinary Tract Infections Than Men
What are the symptoms of fibroids in the uterus?
Many people who have fibroids have no symptoms and may never know they have one or more until a gynecologist performing a routine check-up discovers the growths.
However, according to multiple sources, other people with uterine fibroids may experience the following symptoms:
- Heavy bleeding during periods (enough to cause anemia)
- Periods that last longer than a week, or bleeding between periods
- Menstrual pain
- An extended lower abdomen
- Abdominal cramps or pain
- Pelvic pressure, pelvic pain, or a feeling of fullness in the lower abdomen
- Lower back pain
- Leg pain
- Pain during sex
- Frequent need to urinate, or, difficulty urinating to completion
- Constipation, or difficulty with bowel movements
- Fertility problems (rare)
These symptoms, depending on their severity, can make life very difficult and painful for people who experience them. In a 2018 survey of French women who had uterine fibroids, 64% of respondents reported fibroid symptoms had a “moderate to very important” effect on their quality of life.
Who is at-risk for uterine fibroids?
Anyone with a uterus is at risk for uterine fibroids — but some more than others. The likelihood of developing uterine fibroids increases with age, until menopause; due to hormone changes, developing new uterine fibroids after menopause, while possible, is less common.
Uterine fibroids are also more common among people with relatives who have had uterine fibroids, suggesting a genetic component. Uterine fibroids are also more common among African-American women than other ethnicities, including South Asian.
Some research suggests people whose first period came at an earlier age may be more at risk for uterine fibroids.
Finally, other studies suggest repeat pregnancy offers a protective effect, as risk of fibroids lowers across each pregnancy.
Several other lifestyle factors — from obesity to use of hormonal contraception — have been linked to higher or lower risk of uterine fibroids, but research in these areas has been inconclusive.
Related on The Swaddle:
What happens when you develop uterine fibroids during pregnancy?
It’s common to develop uterine fibroids for the first time, or develop a new growth, during pregnancy, a time when hormones are fluctuating wildly. “This doesn’t mean there will be problems. Most women with fibroids have normal pregnancies,” according to the U.S. Department of Health and Human Service’s Office on Women’s Health.
That said, people with fibroids during pregnancy are six times more likely to require a C-section delivery. Other potential pregnancy complications related to fibroids include: restricted fetal growth, placental abruption (when the placenta detaches from the uterus before delivery, threatening the baby’s supply of oxygen and nutrients), and preterm birth.
Can uterine fibroids keep you from getting pregnant?
It’s unlikely. Uterine fibroids can affect fertility, but it’s a rare occurrence, and seems to be related to location of the growths than anything else. A 2016 review of research into uterine fibroids and fertility suggests submucosal fibroids — fibroids that bulge or hang into the uterine cavity — may affect conception; intramural fibroids (growths within the uterine wall) and subserosal fibroids (growths that bulge or hang toward the exterior of the uterus) had little-to-no relation to fertility. Ultimately, however, “the evidence regarding effect of fibroids on infertility and reproductive outcomes is weak and mostly inconclusive,” concluded the review.
What are the risks or complications of uterine fibroids?
Aside from the potential impairment to quality of life, there are few health risks or complications from fibroids. For people who experience heavy bleeding related to fibroids, anemia could be a health risk. And in the rare case that a fibroid grows very large, pressure on the bladder and urethra can cause kidney damage, according to UCLA Health.
Do uterine fibroids increase cancer risk?
No. Uterine fibroids have no association with the risk of any cancer.
However, while uterine fibroids are benign tumors, very rarely, a cancerous growth in the uterine wall may occur. This is called a leiomyosarcoma, a type of malignant tumor that could develop in any of the body’s muscle or fat tissues or blood vessels, not just in the uterine wall. “Doctors think that these cancers do not arise from an already-existing fibroid. Having fibroids does not increase the risk of developing a cancerous fibroid,” according to the U.S. Office on Women’s Health.
How are uterine fibroids diagnosed?
Most people don’t know they have fibroids until they visit a gynecologist for a routine physical check-up, or undergo a prenatal ultrasound. Confirmation may come via other tests, such as: a transvaginal ultrasound (sometimes with saline pumped into the uterus), an MRI, or a hysteroscopy, a surgical procedure in which a scope is inserted into the uterus.
Do uterine fibroids require treatment?
If you have uterine fibroids, but no-to-few/light symptoms, most doctors will say no treatment is necessary.
“I consider the severity of symptoms and the impact of those symptoms on a woman’s quality of life to be the foundation of treatment decision making,” Dr. Aaron Styer, an obstetrician-gynecologist at Harvard-affiliated Massachusetts General Hospital, told Harvard Health Publishing. “For example, is the woman missing work, requiring frequent hospitalizations, or missing out on normal, daily life? If so, that information will guide the treatment I recommend.”
However, most doctors will also advise ‘Watchful Waiting‘ in best-case scenarios with no symptoms — that is, monitoring fibroid growth and symptoms through regular abdominal and/or pelvic exams.
What uterine fibroid treatments exist?
For anyone with more severe and impairing fibroid symptoms, there are a few options for fibroid management and/or removal. The only total and lasting cure for fibroids, however, is a hysterectomy. Since a hysterectomy is a major surgery that removes the uterus, it carries its own risks, and it’s not a first-line treatment for fibroids; many experts do not consider it a treatment at all, unless a person has already had children and/or is past childbearing age.
People with severe uterine fibroids, then, have several treatment options, per UCLA Health:
- Medication. This typically takes the form of low-dose hormonal birth control or other hormone-regulating medications. This line of treatment aims at alleviating symptoms.
- Uterine fibroid embolization. An alternative to surgery, this minimally invasive procedure involves blocking the blood flow to fibroids, which causes them to shrink in size. This procedure may need to be repeated, if the blocked fibroids resume growth, or new ones develop.
- MRI-guided focused ultrasound. This completely non-invasive treatment focuses concentrated sound waves on a targeted fibroid, heating it to the point of cell death without damaging any surrounding tissue, a process known a thermal ablation. This procedure destroys targeted fibroids, but does not prevent new ones from growing.
- Surgical removal. Various types of surgeries are possible to remove fibroids. However, new fibroids can grow after the surgery.
A doctor can advise on which line of treatment is most suitable and available.
Liesl Goecker is The Swaddle's managing editor.
Related

Suppressing Thoughts, Needs, and Emotions in Relationships Is Linked to Risk of Stroke for Women