
Everything You Need to Know About Vaginal Yeast Infections
Learn the causes, signs and treatment of the infection that 3 in 4 women will get at some point in life.
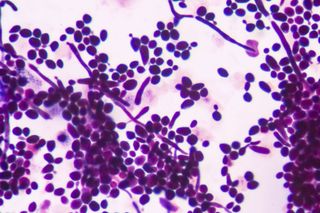
A vaginal yeast infection — also called vaginal candidiasis — occurs when the yeast fungus (candida) that is naturally present in the vagina’s microbiome (the collection of good bacteria, fungi, and other microbes that help keep the vagina self-cleaning and healthy) proliferate beyond normal amounts. The imbalance can cause discomfort and pain — it may also itch ‘down there’ — but it’s not typically considered a serious health risk. Still, here’s what you need to know to live your life through the irritation and soreness.
What causes a yeast infection?
The fungus Candida albicans is behind most yeast infections. It’s a naturally occurring microbe in the vaginal microbiome that can proliferate out of control when other microbes diminish. (That said, other types of yeast can cause yeast infections, too, but it’s rarer.)
Certain activities can aid this imbalance. Douching, contrary to popular belief, is an entirely unnecessary, unhygienic practice that actually disrupts the balance of the vagina’s microbiome, makes the vagina less healthy, and puts individuals at risk of a vaginal infection. Excess use of antibiotics — for instance, taking antibiotics for a cold or the flu (for which antibiotics are ineffective) — can kill off the kinds of vaginal bacteria that hold yeast microbes in check and contribute to a yeast infection. Hormone fluctuations — as associated with pregnancy, hormonal birth control use, and/or hormone therapy — can also affect the balance of the vagina’s microbiome and cause a vaginal yeast infection.
The bottom line is this: Yeast infections aren’t caused by being dirty. They’re caused by a host of factors, many entirely natural and many outside the control of the person experiencing one.
Who gets yeast infections?
Three in four women will get a yeast infection at some point in their lives; many of them will experience at least two. Pregnant women are particularly prone to yeast infections, for the same reason they are more prone to urinary tract infections: their hormonal fluctuations can alter the balance of the vagina’s microbiome. For the same reason, women who use hormonal birth control may also be at higher risk for yeast infections.
That said, anyone with a vagina is able to contract a vaginal yeast infection. And anyone, period, is able to contract a yeast infection in other parts of the body. (For instance, a yeast infection of the mouth is known as thrush, and yeast infection is a major cause of diaper rash in babies.)
Are yeast infections contagious?
A yeast infection is not considered a sexually transmitted infection, because people with vaginas can also develop a yeast infection by other means than sex. That said, according to the Mayo Clinic, some research suggests that sexual intercourse — both oral and vaginal — can affect one’s risk of yeast infection. Still, “it isn’t quite clear to scientists whether having oral or vaginal sex when you have a yeast infection makes your partner more likely to get a yeast infection as well,” according to Planned Parenthood.
Either way, experts are quite clear: It’s best to avoid vaginal and/or oral sexual activity until the yeast infection has cleared up — partly because they’re not 100% sure if the infection transfers to a partner, partly because the friction of sex can irritate the vaginal tissue further and worsen the infection, and partly because some oil-based yeast infection treatments could cause condoms to break, raising the risk of pregnancy.
Related on The Swaddle:
Why Women Are More Prone to Urinary Tract Infections Than Men
What are the symptoms of a yeast infection?
According to Planned Parenthood and the Mayo Clinic, typical yeast infection symptoms include some or all of the following:
- thick, white, chunky discharge that is often described as akin to cottage cheese and typically has no different odor than normal
- watery vaginal discharge that typically has no different odor than normal
- itching, burning, soreness or pain around the vagina and vulva
- burning during sex or while peeing
- a reddened or swollen vulva
- a vaginal rash
- a creamy, whitish coating in or around the vagina
- tears, fissures or sores on the tissue in and around the vagina and vulva (extreme cases only)
Why are yeast infections common before and after periods?
Yeast infections are common before and/or after periods for the same reason pregnant women and women who use hormonal contraceptives are more prone to developing yeast infections: hormonal fluctuations. The waxing and waning of hormones around the time of menstruation can also alter the balance in the vagina’s microbiome and put someone at risk of a yeast infection.
What happens if I have a yeast infection and my period at the same time?
Nothing. Yeast infections are treatable during menstruation. Also, “it’s totally fine to use tampons or pads if you’re bleeding and also have a yeast infection,” Dr. Jennifer Conti, a clinical assistant professor at Stanford University in obstetrics and gynecology, told Women’s Health in 2017. However, (a) make sure they are not scented, or deodorizing, tampons and/or pads, which could contribute to an imbalanced vaginal microbiome, and (b) anyone menstruating and experiencing a yeast infection at the same time might want to be more conscious about frequently changing tampons or pads.
Do I need to see a doctor for a yeast infection?
For anyone who has never had a yeast infection before, it is a good idea to consult a doctor to confirm the diagnosis before attempting to treat a yeast infection at home. Also, pregnant women, women who have diabetes, women who have a weakened immune system, and women who have had four or more yeast infections in the last year should consult a doctor for treatment automatically.
However, for anyone else who is familiar with yeast infections and recognizes the signs, many over-the-counter treatments are available.
What is the treatment for a yeast infection?
According to the Mayo Clinic, anti-fungal medication for yeast infection can come in a variety of forms: creams, ointments, oral pills, and vaginal suppositories. Regimen differs according to each medication, and treatment can last anywhere from one day to a week. Oral pills are not recommended for pregnant women.
For severe yeast infections, or lingering symptoms, a doctor might prescribe a longer course of anti-fungal therapy, a multi-dose therapy (two or more different kinds of anti-fungal medications), or, as a last recourse, a boric acid vaginal suppository, if the infection proves resistant to other forms of treatment.
Can home remedies cure a yeast infection?
Home remedies for yeast infection are popular; a quick Google search will provide lists upon lists of at-home, DIY yeast infection treatments, with dahi (yogurt) topping recommendations. While some of these jugaad remedies have tentative or inconsistent scientific support for their curative effects, none have been tested remotely enough to be considered actual treatments. Experts are clear: Do not attempt an at-home, DIY remedy for a vaginal yeast infection without consulting a doctor first.
Can I do anything to prevent a yeast infection?
Yes, certain measures can minimize one’s risk of a vaginal yeast infection, per the Mayo Clinic. Avoiding douching tops the list of preventative actions. And avoiding scented feminine products, including pads and tampons, is also a good step for the same reason; the scent additives can disturb the balance of vaginal microbes.
Also, avoiding unnecessary antibiotics can prevent the kinds of vaginal bacteria that hold yeast microbes in check from dying off.
Finally, avoiding lingering in damp clothes, especially damp clothes made of synthetic material — such as swimsuits, workout clothes, pantyhose, and synthetic underwear — can do much to minimize the chances of a yeast infection. Note that it’s the breathability of the fabric that is as important as the dryness; for instance, using talcum or other powders might avoid vaginal dampness, but it’s definitely not a good idea for vaginal health.
Liesl Goecker is The Swaddle's managing editor.
Related


The Vagina Is Perfectly Capable of Cleansing Itself, No Douching Required
