Why Rabies Continues to Be a Problem in India Despite Being Preventable
India accounts for 36% of all global rabies deaths.
India held its first Rabies Awareness Summit on World Rabies Day on September 28 this year, to demand the government take drastic, persistent steps to eradicate rabies specifically by dog bites in India. In order to meet the World Health Organization’s target of eradicating rabies globally by 2030, experts at the summit advised the Indian government to make rabies a “notifiable disease” (required by law to be reported to government authorities to foster accurate record-keeping) like polio, to ensure the disease gets the attention and resources it has so far lacked, especially in rural areas stricken with poverty in the country.
Rabies is a vaccine-preventable disease. India accounts for 36% of all rabies deaths globally, reporting approximately 20,000 cases a year, according to the National Health Portal. These statistics have remained the same for more than a decade, the World Health Organization states, which signals a lack of dedicated resources assigned to fight the virus. This fight is especially important because it is close to impossible to recover from the disease once symptoms set in — rabies is the only disease that has a 100% fatality rate in India. Prevention, experts say, is everything.
How rabies affects the body
Rabies spreads from certain animals — typically dogs, but also cats, bats, and mongooses — to humans via bites and scratches. Once bitten, symptoms typically appear sometime between one and three months later. In rare cases, symptoms may manifest as quickly as one week or as delayed as one year.
Rabies symptoms mimic those of the flu initially, including weakness, fever, and headache. The bite can also cause a prickling or an itching sensation at the site. The virus, as it travels from the bite to the brain, can then cause anxiety, confusion, and cerebral dysfunction, according to the U.S. Centers for Disease Control. At late stages, people infected with rabies can experience hallucinations, delirium, insomnia, and an uncharacteristic fear of water. Once these signs appear, rabies is typically fatal.
Related on The Swaddle:
Nagaland’s Dog Meat Ban Is an Exercise in Bias, Not Animal Rights
The standard treatment for rabies is washing wounds with soap and water, administering rabies immunoglobulins that work as antibodies against the virus, and is followed up by a course of rabies vaccines that provide long-term immunity. Despite these treatment options, it is immensely difficult to recover from a rabies infection once it has firmly been established in the body — only a handful of people around the world have ever survived a rabies infection. Hence, without any real ‘cure’ available, experts around the world agree prevention using vaccination — both pre- and post-exposure — is the only way to fight against rabies.
Why rabies is a problem in India
Maneka Gandhi, minister of women and child development and animal welfare activist, added, “Eradicating rabies will take a sustained program like the one we have for polio, so that measures can be monitored and evaluated. It requires vaccination and sterilization of dogs, but the political will for all this is largely missing.”
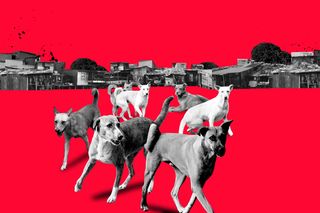
Addressing rabies boils down to addressing three problems. The first arises out of the animals themselves — globally, 97% of rabies cases are caused by dog bites. In India, rabies cases mainly come from a large and unvaccinated stray dog population. India’s stray dog population is currently estimated to be between 35 and 40 million, sustained primarily by dog lovers in the country who deign to feed them. However, nobody is institutionally responsible for vaccinating these dogs, made all the more difficult by the fact that they’re not trained and quite difficult to get a hold of in large numbers.
This issue has alarmed animal rights activists in recent years, complicating rabies control. Without a proper framework to handle a large number of stray dogs — largely considered a nuisance — residents around the country have taken the matter into their own hands, often through illegal means that entail bribing dog catchers and asking them to remove stray dogs from their neighborhood. This has resulted in the disappearance of a large number of stray dogs, from South India, for example, which activists fear means either the dogs were poisoned, or picked up and dropped in a different locale, which reduces their chances of survival. The WHO has said these kinds of surreptitious practices make no dent in the fight against rabies, and what is needed instead is an ethical framework of animal birth control programs that foreground both the animal and human rights in the process.
The second problem we run into in India is a lack of awareness about rabies, and more importantly, lack of knowledge around its prevention and treatment. According to a 2006 study published in the Journal of Communicable Diseases, only 70% of people in India had ever heard of rabies, and a mere 30% of whom knew they should wash the wound after being bitten. The study also found only 60% of people who got bit received prophylaxis and an effective vaccine. The other (faulty but pervasive) treatment options included applying chilies, turmeric, lime, kerosene oil, or herbal paste to the wounds, or consulting an occult practitioner for alternative healing options. The study found fear of injections, the requirement of multiple visits to anti-rabies clinics, and expensive treatment as the reasons for widespread adherence to dangerous, inefficient treatments.
And finally, a third problem lies in the very infrastructure in Indian healthcare dedicated to fighting rabies. On paper, the government has a “National Rabies Control Programme” (NRCP), in effect since 2013, entrusted with educating people about canine rabies and providing pre- and post-exposure vaccination options free of cost. However, a 2017 survey of rabies in India shows it has been largely ineffective, mainly due to a lack of funds. The survey found basic antiseptic facilities for cleaning out dog bites and the availability of rabies immunoglobulins — antibody medication given to rabies victims following exposure, that should be followed up by a course of rabies vaccine — present only in 19 out of 35 anti-rabies clinics, called ARCs(spanning seven states). Researchers also found in 18.4% of the government ARCs, the rabies vaccine was out of stock, and not replenished.
The survey, as have many before it, concluded: “that rabies vaccine was … interrupted in the public sector, particularly in rural areas.” While rabies treatment options were more continuously available in private hospitals, researchers found the high cost of said treatment did not fill the gap, particularly for poverty-stricken populations found to be disproportionately affected by rabies. For now, the disease stays neglected because “it is a disease of the poor,” Dr. M.K. Sudarshan, founder of the Association for Prevention and Control of Rabies in India, told The Guardian.
Rajvi Desai is The Swaddle's Culture Editor. After graduating from NYU as a Journalism and Politics major, she covered breaking news and politics in New York City, and dabbled in design and entertainment journalism. Back in the homeland, she's interested in tackling beauty, sports, politics and human rights in her gender-focused writing, while also co-managing The Swaddle Team's podcast, Respectfully Disagree.
Related


Watching Nature Programming Can Boost Well‑Being, Says Study