A Greek woman with a history of infertility on Tuesday gave birth to a baby conceived using DNA from three people, paving the way for the IVF procedure to aid women who struggle to get pregnant. Both mother and baby are reported to be in good health.
The birth resulted from a clinical trial to assess the efficacy of using mitochondrial replacement therapy (MRT) — more commonly known as ‘three-parent IVF’ — to treat infertility, and could revolutionize options for women struggling to get pregnant.
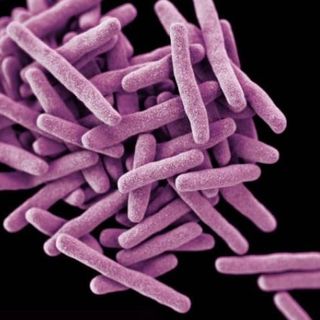
Three-parent IVF involves taking the nucleus of the mother’s egg, and inserting it into a donor egg whose cell nucleus has already been removed. The resulting hybrid egg — which contains the mother’s nuclear DNA and the donor’s mitochondrial DNA — is then fertilized with the father’s sperm, and the embryo transferred into the mother’s uterus. Mitochondrial DNA determines metabolic fitness only; nucleic DNA determines nearly everything else, including physical appearance. The technology was developed to prevent deadly, heritable mitochondrial diseases, but now appears useful in aiding women with a history of infertility. The woman who gave birth Tuesday, before entering the trial and becoming pregnant, had undergone two operations for endometriosis and four unsuccessful cycles of IVF.
The 32-year-old is not the first person to become pregnant and give birth following mitochondrial replacement therapy; a Jordanian woman in 2016 was. But in the latter’s case, and in all other cases until now, MRT was used to prevent mitochondrial disease. This is the first proof that it may be valuable in treating infertility, too.
But the procedure remains controversial. The U.K. became the first country to approve MRT in 2015, but only when there’s a high risk of serious mitochondrial disease. The U.S. has effectively banned the procedure since the same year, when it prohibited its regulatory agency from approving for clinical trial any therapy that intentionally creates or modifies human embryos.
In India, mitochondrial replacement therapy exists in a relatively unregulated gray area. A study last year found two clinics in the country advertising cytoplasmic transfer (CT), an early version of the technique with questionable results; CT was banned by the U.S. in 2001 after it was linked to developmental disorders in babies born from embryos that had undergone the procedure. Follow-on research has yet to confirm the link, and CT is still available in many countries.
In a statement, Nuno Costa-Borges, co-founder of Embryotools, one of the labs running the trial, touted the success of the trial, “Our excellent collaboration and this exceptional result will help countless women to realize their dream of becoming mothers with their own genetic material.”