All You Need to Know About Preeclampsia During Pregnancy
The pregnancy complication affects roughly 1 in every 20 pregnancies in India.

Preeclampsia during pregnancy is a complication that affects roughly one in every 20 pregnancies in India. Unfortunately, science hasn’t managed to crack it; despite recent, promising advances in research, no measures can prevent preeclampsia, and diagnosis of the complication is inexact — occurring only once the condition takes a serious turn.
What is preeclampsia during pregnancy?
Preeclampsia occurs when a pregnant woman has unusually high blood pressure that impairs the proper function of her organs, typically her kidneys and liver. It does not typically manifest before 20 weeks’ gestation, and in rare cases can even develop after birth, during the fourth trimester. While it’s a serious condition, the good news is if it’s spotted early and managed with prenatal care, most women can still deliver a healthy baby.
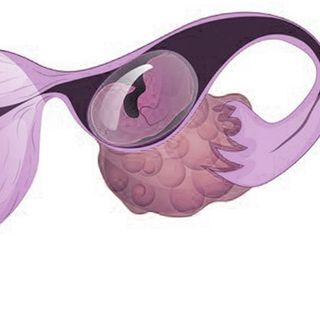
Despite the fact that it doesn’t manifest until the second half of pregnancy, the roots of preeclampsia are laid during early gestation. At its most basic, preeclampsia boils down to a problem in the formation of the blood vessels within the placenta. In preeclamptic women, placental blood vessels are narrower and don’t function properly in response to the hormonal fluctuations of pregnancy. There is some evidence that a baby’s DNA might contribute to the development of preeclampsia, since placental development is prompted by fetal DNA — itself a combination of parents’ genes, and preeclampsia is known to run in families of both women and their male partners. Immune disorders may also contribute to the poor formation of placental blood vessels.
Related on The Swaddle:
Your Pregnancy Diet Can Ease Side Effects, Prevent Complications
What are the symptoms of preeclampsia?
The first sign of preeclampsia is elevated blood pressure; an OB/GYN will monitor a pregnant woman’s blood pressure at each prenatal checkup. In some cases, for women at risk of preeclampsia, doctors may ask a pregnant woman to track her blood pressure at home.
Blood pressure higher than 140/90 recorded twice, with at least four hours between the recordings, is evidence of preeclampsia. Other accompanying signs include the following; a woman should contact her OB/GYN or go to a hospital immediately if she experiences:
- Sudden weight gain and/or swelling of the face and hands (sudden being the keyword, as swelling can also be a generic side effect of pregnancy)
- Persistent headache
- Blurry vision, seeing spots, sensitivity to loss, temporary loss of vision, or any other sudden vision change
- Abdominal pain, typically located on the right side, under the ribs
- Nausea or vomiting
- Shortness of breath (caused by fluid in the lungs)
- Decrease in urination
An OB/GYN or hospital will also be able to check for the following signs:
- Urine containing excess protein, and other signs of poor kidney function
- Low blood platelet levels
- Signs of poor liver function
Who is at risk for preeclampsia?
Preeclampsia can develop even in women with normal blood pressure. The following list includes risk factors for preeclampsia:
- A family history — if there is a history of preeclampsia among the woman’s family or her partner’s family, the risk of preeclampsia increases.
- Chronic high blood pressure — if a woman has high blood pressure before pregnancy, she’s more likely to develop preeclampsia.
- A first pregnancy — preeclampsia risk is highest among women during their first pregnancy. However, preeclampsia risk is also higher for people on their second pregnancy if it’s been less than two, or more than 10 years, since their first pregnancy. A second or third pregnancy with different paternal genes from the first one(s) also increases risk.
- Previous bout of preeclampsia or gestational hypertension – a previous pregnancy characterized by either of these conditions can increase risk.
- Age – very young expectant mothers, and expectant mothers above 40 are more at risk of developing preeclampsia during pregnancy.
- Obesity
- Pregnancy with multiples — with twins, triplets or multiples all carry greater risk of preeclampsia.
- Preexisting conditions — including chronic high blood pressure, migraines, diabetes types 1 and 2, kidney disease, blood clots, and lupus, all increase risk of preeclampsia.
- IVF — conception via assisted reproductive technology increases the risk of preeclampsia later.
What is the treatment for preeclampsia?
The best treatment for preeclampsia, for both mother and baby, is delivery, since the progression of the condition can be fatal for each. However, if preeclampsia develops before a baby can survive outside the womb, and is caught early when symptoms are mild, a doctor may be able to manage the condition until the baby is fully developed. At this point, doctors may advise the following: consume less salt and more water, bedrest reclining on the body’s left side, diet changes, and other behaviors.
What are the effects of preeclampsia?
For mothers, if preeclampsia is not spotted and treated in time, the pregnancy complication can cause liver failure, kidney failure, or long-term cardiovascular problems in the future. Severe preeclampsia can also develop into eclampsia, which can cause seizures and death, or HELLP syndrome, which is characterized by impaired liver function and clotting problems.
For babies, preeclampsia can cause low birth weight. Since the placenta is the fetus’s main source of nourishment, problems with blood flow through it can keep the baby from receiving enough blood and oxygen to develop properly.
Liesl Goecker is The Swaddle's managing editor.
Related


Women Recall Their First‑Period Experiences