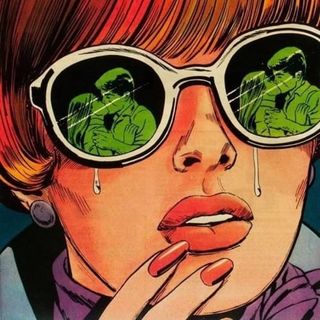
Benefits of New Ketamine‑Based Antidepressant Drug Outweigh Risks, Experts Say
Unlike other antidepressants, it takes mere hours to kick in.

The first breakthrough in pharmaceutical research for depression since the launch of Prozac in the 1980s has come in the form of a club drug. Esketamine, a ketamine-based antidepressant, takes effect in mere hours, unlike other medication, which can take weeks or months to kick in.
Approved by the U.S. Food and Drug Administration on 5 March, esketamine, in the form of a nasal spray, will be used to treat drug-resistant forms of depression. While ketamine has been used intravenously on some depression patients since the 2000s, the costly and experimental injections weren’t covered by insurance. The new approval of esketamine, a molecule derived from ketamine, means pharmaceutical companies will be able to sell the drug at a lower price, so it can reach more people.
But some experts have concerns about how quickly the drug was approved and its potential risks.
Most other depression medications target the brain’s production of serotonin, norepinephrine, and dopamine — chemicals that act as neurotransmitters, ferrying messages between neurons. Esketamine is the first drug to target the brain’s glutamate pathways instead, which are thought to strengthen synapses in the brain’s frontal cortex, an area that is responsible for controlling mood and motivation. For many psychiatrists and tpatients involved in the clinical trials, the drug has seemed miraculous, as patients feel its effects in a couple of hours.
“The approval of esketamine will be a sentinel event for patients with depression,” commented Walter Dunn, a psychiatrist at UCLA and member of the panel that recommended the drug’s approval. “The findings of rapid onset and efficacy in treatment-resistant depression weren’t surprising, given our experience with off-label use of [intravenous] ketamine,” Dunn added. “What was less clear — and of significant importance — was if patients who improved on esketamine could remain depression-free long-term taking esketamine.”
And this is a big question, since the entire process for esketamine to get approved was expedited by an industry eager to see groundbreaking progress in the treatment of depression.
Related on The Swaddle:
Do Antidepressants Affect Fetal Development?
After the promising early, unregulated evidence of the drug’s effectiveness, the FDA designated it as “breakthrough therapy,” granting it priority review, which shortened the approval process to six months. Two Phase 3 trials for the drug showed significant results: a 50 percent success rate for a reduction in depression symptoms, as well as a lowered risk of relapsing after withdrawal. However, this was out of a total of five trials at that stage; the other three Phase 3 trials did not show statistically significant results.
Researchers are also concerned with the approval of a drug that has hallucinatory and dissociative, or out-of-body, effects. Julie Zito, a pharmacy professor and one of the members of the panel who voted against the drug’s approval said, “I can’t imagine that there are no consequences to having had a bad experience from dissociation — like hallucination, confusion, or lack of awareness of your surroundings. And when you’re talking about some individuals who have an impulse for suicide, then I begin to worry: What happens when the drug is not helping them?”
The trials were conducted in a controlled clinical environment, and although randomized to check for effectiveness, the sample sizes ranged from only 100 to 700 — not nearly enough to convince some experts of its efficacy among larger populations. Experts also aren’t sure what the possible long-term effects of the drug might be, since this is a fairly recent innovation in the field.
Sill, most researchers and psychiatrists agree the benefits of this treatment for medication-resistant patients who would otherwise have no recourse, far outweigh these concerns. Esketamine’s manufacturer Janssen Pharmaceuticals, a subsidiary of Johnson & Johnson, is working with the FDA towards risk and mitigation strategies to ensure the drug will not be abused, since ketamine does have the potential for addiction. For instance, esketamine dose must be administered only by a doctor who will monitor patients for the potential dissociative side effects.
Testing is now underway for esketamine’s potential use for other mental health issues like bipolar disorder. In the end, “it’s always a matter of judgement and opinion,” argues David Hough, a psychiatrist who led the clinical trials for Janssen Pharmaceuticals, at Johnson & Johnson. But the overwhelming consensus among researchers seems to be that this drug is a game changer. With these groundbreaking innovations in the field, hopefully depression patients in India too will be able to avail of this medication sooner rather than later.
Nadia Nooreyezdan is The Swaddle's culture editor. Since graduating from Columbia Journalism School, she spends her time thinking about aliens, cyborgs, and social justice sci-fi. She's also working on a memoir about her family's journey from Iran to India.
Related

Shame, Family Secrecy Lead to Mishandling of Child Sexual Abuse
