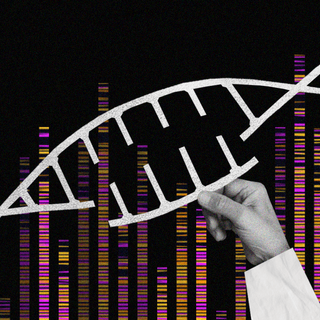
The human immunodeficiency virus (HIV) is among the world’s most notorious maladies that don’t have a cure — yet. According to new research, the clustered regularly interspaced short palindromic repeats (CRISPR) is a gene-editing tool that could intervene now to change that. The technology involved worked like this: CRISPR identifies genes in the human blood that play a role in allowing HIV virus to replicate in the body. Pinpointing the disease to this level of precision could lead to curative therapies in the future.
The implications of the study, published in Nature Communications last weel, are huge. CRISPR effectively provided a “map” of HIV interactions with host T-cells. “Human Immunodeficiency Virus (HIV) relies on host molecular machinery for replication… we target 426 genes previously implicated in the HIV lifecycle… in order to systematically assess their functional roles in HIV replication,” the paper noted.
Related on The Swaddle:
An Existing Cancer Drug Could Help Cure HIV One Day, Find Scientists
Researchers at Northwestern University looked at 86 genes — with 40 never having been associated with HIV before — as being involved in the way HIV infections take place. Scientists have previously used immortalized cancer cells to study the same, Science Daily noted.
CRISPR, however, allowed them to understand HIV as it spreads in the human body by “turning off” certain genes to test their impact on the virus’s replication. “This capability to turn genes on and off in cells isolated directly from human blood is a game changer — this new assay is the most faithful representation of what’s happening in the body during HIV infection that we could easily study in the lab,” said Judd Hultquist, a co-corresponding author of the study.
Related on The Swaddle:
We’re One Giant Leap Closer to an HIV Vaccine
In the experiment, T-cells — a type of immune cell targeted by HIV — were isolated from human blood, with some cells having had hundreds of genes “knocked out” or “turned off” by CRISPR. Scientists then infected these cells with HIV to analyze the response: while some cells without certain genes showed decreased infection, some with antiviral cells that were knocked out showed increased infection. This method allowed researchers to identify exactly which genes propagated the spread of infection, and which ones inhibited it.
A part of the experiment validated what scientists already knew, but the other half identified new pathways of infection through genes that weren’t previously associated with HIV. “That nearly half of the genes we found were previously discovered increases confidence in our dataset. The exciting part is that over half — 46 — of these genes had never before been looked at in the context of HIV infection, so they represent new potential therapeutic avenues to look into,” Hultquist added.