Minimally Invasive Surgeries For Early Stage Cervical Cancer Have Lower Survival Rate Than Open Surgeries
It depends on how good your surgeon is, experts say.
A new study by researchers from Columbia University may have doctors reconsidering their line of treatment for early-stage cervical cancer patients.
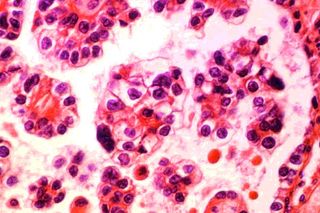
They found that women in the early stages of cervical cancer who underwent radical hysterectomies with minimally invasive surgery had a 65% higher risk of death than those who had open surgery. The results were based on comparisons between the same operation, radical hysterectomy, performed both as open surgery and as a minimally invasive procedure.
Radical hysterectomy is the removal of uterus, cervix and other parts of the female reproductive system. A radical open surgery, as the name implies, is done through a large, open cut in the skin while minimally invasive surgery would mean making smaller incisions either with a laparoscopic, or keyhole, procedure (when doctors use a tiny camera to view the area and small tools to perform the surgery) or a robot-assisted procedure (when surgeons use a high-tech precision robot rather than their hands).
The study, published in the New England Journal of Medicine, said that although researchers have always suspected that there could be a difference in survival between the two approaches, “…the extent of the difference was surprising,” said co-principal investigator Dr. Jason D. Wright, an associate professor of obstetrics and gynecology at Columbia University’s Vagelos College of Physicians and Surgeons. “Our findings suggest that minimally invasive surgery may not be appropriate for many patients with early-stage cervical cancer.”
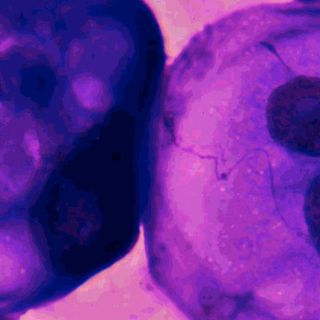
According to statistics available with the department of health and family welfare, cervical cancer accounts for 26% of female cancers in India, and accounts for 17% of all cancer deaths among women aged 30 and 69 years old. It is said to occur in every 1 in 53 Indian women — as compared to 1 in 100 women in more developed regions of the world. In the US, 13,000 women are diagnosed with cervical cancer each year.
The researchers analyzed data from US-based National Cancer Database of 2,461 women with early cervical cancer who underwent radical hysterectomy between 2010 and 2013. Within four years of the surgery, 9.1% of those who had undergone minimally invasive surgery had died versus 5.3% in the open-surgery group.
Wright and his colleagues also analyzed information from a separate national cancer database and found a stable four-year survival rate for early-stage cervical cancer prior to 2006, when most doctors in the US started adopting minimally invasive procedures for early-stage cancer patients. However, “survival began to decrease after then — exactly the same time that some surgeons began performing minimally invasive hysterectomies,” Wright said.
This trend suggests a cause-and-effect relationship between minimally invasive procedures and lower survival rates, but why does it happen?
Dr Amit Gandhi, an oncosurgeon at Mumbai’s Tata Memorial Hospital says, “Minimally invasive surgery is not inherently inferior to open surgery, but one possibility of a higher death rate associated with it could be that the surgeons who performed minimally invasive surgery on patients in this study may have been more experienced with open surgery.” He adds, “Even from my experience, I can say that a lot depends on the surgeons.”
Agrees Dr Manoj Lokhande, a surgical oncologist at Onco-Life Cancer Centre. “I’ve performed over a 100 open surgeries but only about 25 minimally invasive ones because the cure rates with open surgeries are better and survival rates higher,” says Dr Lokhande. “Besides, open surgeries have more advantages — they are cheaper, need only local anesthesia, as opposed to a general one in minimally invasive hysterectomies. Only a surgeon with a lot of experience in minimally invasive surgeries should be trusted.”
Another possible explanation for the disparate survival rates associated with each type of surgery, according to Wright, is that uterine manipulators, which are used to retract and visualize the pelvic area during minimally invasive hysterectomy, may inadvertently end up spreading microscopic tumor cells.
“We recommend that patients talk to their doctor about the available surgical options,” Wright says. “Although minimally invasive surgery was associated with higher mortality, some patients may be willing to accept that risk, especially if they have very early cancers.”
Despite his findings, Wright says patients who have already undergone minimally invasive surgery should not worry; they may not necessarily need more checkups or more screening.
“The overall prognosis for women with early cervical cancer after minimally invasive or open hysterectomy is excellent,” he adds. “In either case, they should get periodic checkups, and if they experience any symptoms, such as pain or changes in vaginal bleeding, they should consult their gynecologic oncologist.”
Anubhuti Matta is an associate editor with The Swaddle. When not at work, she's busy pursuing kathak, reading books on and by women in the Middle East or making dresses out of Indian prints.
Related

Gratitude Might Be the Secret to Raising a Non‑Materialistic Kid