
New Test Predicts Cervical Cancer With 100% Accuracy
“This is an enormous development.”
Researchers have developed a cervical cancer test that can detect the disease up to five years before it manifests, with 100% accuracy in a randomized clinical trial of more than 15,000 women. However, they also said it could take up to five years for it to become routine procedure in gynecologist’s offices.
“This is an enormous development,” said Attila Lorincz, PhD, a professor at Queen Mary University of London and the lead researcher behind the new test. “We were surprised by how well this new test can detect and predict early cervical cancers years in advance, with 100% of cancers detected, including adenocarcinomas, which is a type of cervical cancer that is very difficult to detect.”
India is home to a quarter of the world’s cases of cervical cancers 1 and 2; here, the disease accounts for 26% of all cancers in women, and 17% of their cancer-related deaths. Cervical cancer screening efforts have been disjointed, and reliant on the invasive Pap smear to identify cellular mutations, as well as a test for the human papillomavirus virus, an infection that indirectly underlies the majority of the world’s cervical cancer cases. Neither test is foolproof, with Pap smears detecting only around 50% of precancerous cells, and the HPV test only detecting a past or present infection, but not whether it will develop into cancer. The HPV vaccine, despite its proven efficacy in preventing the infection that underlies most cervical cancer cases — and thus lowering the rate of cervical cancer — has been adopted only slowly, as part of public health campaigns in Punjab and Delhi, but not at the national level.
Related: More Evidence HPV Vaccine Is Critical to Preventing Cervical Cancer
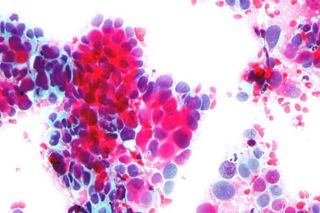
The new test detects naturally occurring chemical markers that overlay DNA that’s been affected by HPV infection, to predict cervical cancer before it develops. It reflects a new trend in cancer research and treatment, one that sees the pantheon of diseases primarily as the result of epigenetics — that is, how, when and why a body ‘reads’ and carries out genetic blueprints. Nessa Carey’s The Epigenetics Revolution explains it best: if each of our lives are a movie, our cells are the actors, genetics is the script — and epigenetics is the directing.
“In contrast to what most researchers and clinicians are saying, we are seeing more and more evidence that it is in fact epigenetics, and not DNA mutations, that drives a whole range of early cancers, including cervical, anal, oropharyngeal, colon, and prostate,” Lorincz said.
In the clinical trial, the new test detected 100% the invasive cervical cancer cases (a total of eight) that developed among a set of 15,744 women. The women in the trial also underwent Pap smears and HPV testing, which detected 25% and 50% of the cervical cancer cases respectively.
Among a subset of HPV-positive women, the new test was slightly less accurate but still highly efficient, detecting 93% of precancerous cervical lesions, compared to 86% detected by a Pap smear and HPV test combined, and 61% detected by a Pap smear alone.
The authors of the study, published in the International Journal of Cancer, said the new test also has the advantage of being cheaper than a Pap smear.
Liesl Goecker is The Swaddle's managing editor.
Related


Study: Sudokus, Crosswords Don’t Slow Cognitive Decline in Old Age
