
Lupus: the Immune System Malfunction Science Is Yet to Decipher
Everything you need to know about the autoimmune disease we don’t know much about.
Every day, more than 5 million people struggle with lupus, according to the World Lupus Federation. Yet, the autoimmune disease continues to be suitably shrouded in mystery. To date, there is no single test to diagnose it, no way to prevent or cure it, no one set pattern of symptoms, and no definitive answer as to what causes it.
Here’s a primer on what we do know.
What is lupus?
Lupus is a wide-spread, lifelong and potentially fatal autoimmune disease that can affect any body part.
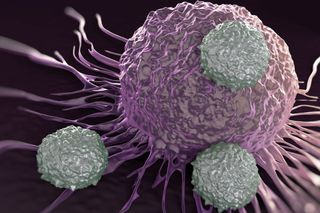
Lupus represents an immune system malfunction. Normally, the body’s immune system produces antibodies that protect the body from ‘invaders,’ like bacteria and viruses. In the case of an autoimmune disease, the immune system is unable to tell the difference between foreign invaders and the body’s healthy tissues, and creates antibodies that attack and destroy the body itself. These antibodies cause inflammation, pain and usually attack the skin, kidneys, joints, blood vessels, heart, and brain in the body.
Lupus also tends to go into periods of ‘flare-ups’ where symptoms increase, and ‘remission,’ where the symptoms temporarily disappear. It is a non-contagious and non-cancerous disease.
What are the different kinds of lupus?
There are four types of lupus:
- Cutaneous Lupus Erythematosus (CLE) that affects only the skin;
- Drug-induced lupus that usually disappears soon after the medication is stopped;
- Neonatal Lupus, a rare condition among infants whose mothers have lupus (though it is not necessary that a mother with lupus will transfer it on to her baby); and,
- Systemic Lupus Erythematosus (SLE) — what we refer to when we colloquially say ‘lupus,’ which targets various organ systems in the body.
What are the symptoms of lupus?
The body inflammation triggered by SLE causes symptoms, which often mimic other less serious illnesses, and range from mild to debilitating. Someone with lupus may experience joint pain, fatigue, photosensitivity, hair loss, a facial rash, arthritis, chest pain, dry eyes, trouble breathing, headaches, confusion, memory loss, and kidney issues, among other symptoms, according to the Mayo Clinic.
How is lupus diagnosed?
Because of the range, extent, and at times, the hide-and-seek nature, of the symptoms, SLE is notoriously hard to diagnose accurately. The symptoms often mimic and can overlap with other ailments such as fibromyalgia, rheumatoid arthritis, and multiple sclerosis, which makes it hard to assess if and when to consider lupus.
To diagnose it, doctors carefully review the patient’s medical history and follow it up with a physical examination and routine laboratory tests such as blood tests, urine tests, and tissue and kidney biopsies. They also run some specialized tests for the immune system, the most crucial one being the ANA test, which detects antinuclear antibodies that attack the body’s tissues. 97% of people with lupus usually test positive for this test, also implying that a negative result for the test does not mean the absence of the condition.
Currently, there is no one test to diagnose the condition.
It can take months or even years for doctors to combine evolving symptoms, physical exams, and test results that sometimes change, to correctly diagnose lupus before severe organ damage occurs.
Who can get lupus?
Anyone.
But, since we don’t know why some people develop lupus, it helps to understand who it typically affects. Nine out of ten people suffering from it are women, especially in the reproductive age group of 17 to 50 years. Within women, African Americans, Hispanics, Asians, and Native Americans top the list with a much higher rate of lupus, according to a 2017 study. Researchers think genes play a role in how it affects minority women; their socio-economic marginalization further increases the condition’s prevalence by restricting access to information and timely and quality healthcare access for treatment.
Only 10% of people with lupus usually have a parent or sibling who has or may develop it; only 5% of the children born to a parent with it develop the illness.
Related on The Swaddle:
Female Immune System Could Hold Key to Fighting Cancer, Autoimmune Disorders
What causes lupus?
We don’t know.
Researchers are still studying what makes the immune system malfunction the way it does in lupus, but have arrived at some factors that play a role in it. While some people may be genetically predisposed to the disease, environmental factors such as a virus, chemicals, infections, ultraviolet light, stress, smoking, and certain medicines may trigger it. In some cases, imbalances in the gut microbiome may drive it.
An international human genetic study also found that one of the genes that increases the likelihood of developing lupus sits on the X-chromosome. Since women have twice as many X-chromosomes than men, this study helps to understand why the condition occurs more frequently in females than in males. Estrogen — known to fortify the immune system — is also linked to lupus because women usually show symptoms before their period or during pregnancy, when estrogen levels are high.
What is the treatment for lupus?
There is no cure.
Treatments are based on the specific needs and symptoms of each person, with the goal to reduce inflammation and maintain bodily functions. To this end, doctors may prescribe low doses of chemotherapy and medication such as nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, antimalarials, and immunomodulating drugs.
With current methods of diagnosis and treatment, 80-90% of people with lupus can look forward to a normal lifespan.
Can lupus be prevented?
No, because we don’t understand its causes fully yet.
For those who already have it, lifestyle changes such as having a good diet, establishing a sleep routine, making regular doctor visits, using sunscreen, getting vaccines to prevent infections, and not smoking can also help prevent periods of ‘flare-ups’ and problems linked to the condition, like kidney disease, osteoporosis, and heart disease.
Pallavi Prasad is The Swaddle's Features Editor. When she isn't fighting for gender justice and being righteous, you can find her dabbling in street and sports photography, reading philosophy, drowning in green tea, and procrastinating on doing the dishes.
Related


Research Links Autism to Higher Than Average Prenatal Hormone Levels
