
Is It Okay to Use Birth Control to Skip a Period (or Several)?
Period-suppressing birth control can benefit women, but its long-term use can lead to health problems.
Monthly periods, while an essential part of women’s reproductive cycles, are often harbingers of pain, mood swings, and societal stigma for the women involved. Periods are also not optional — from a young pubescent girl to a woman approaching menopause, all women are taught that periods are an essential aspect of being able to reproduce, and thus have to be endured every month.
But, what if that’s not totally true?
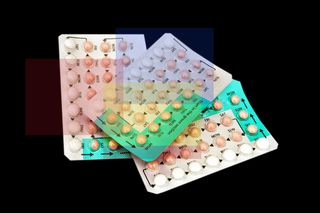
A period-optional movement has been developing in the West, in which women use hormonal contraception — often, birth control pills — to suppress their period by changing hormone levels in their body. The pills suppress the production of progesterone, a hormone that aids ovulation. Low progesterone prevents an egg from being released from the ovary and effectively curbs menstruation. Birth control pills contain various combinations of active hormone pills (that suppress production) and placebo pills (which induce bleeding), taken in timed intervals so they mimic a menstrual cycle, according to the Mayo Clinic. In order to suppress menstruation, women simply skip the placebo pills that induce bleeding, and start the next cycle of active hormone pills.
Newer, extended regimens have also populated medical markets in recent years. Some combinations involve taking the hormone pills every day for three months — effectively preventing periods for that duration — followed by a week of placebo pills and menstruation. Some regimens involve taking active hormone pills that stop all menstrual bleeding for an entire year, according to the Mayo Clinic. In addition to pills, hormonal implants such as certain types of intra-uterine devices, rings and patches can also be used to suppress periods.
Suppressing periods for longer durations has several benefits: It “prevent[s] hormone changes responsible for bleeding, cramping, headaches and other period-related discomforts,” according to the Mayo Clinic. Skipping periods can also be a relief for those with endometriosis, ovarian cysts, menstrual migraines and dysmenorrhea (acutely painful cramps). “For women who experience iron deficiency due to heavy menstrual bleeding, using continuous regimens can reduce bleeding and there is less chance of developing iron deficiency,” according to the Mayo Clinic.
In India, however, period suppression is quite a contested idea — the idea of not getting one’s periods is considered not normal. “The concept of period suppression is very rare. Here, if ladies don’t get their periods, they get very worried,” gynecologist Dr. Aditi Nadkarni said. “For contraception, they take monthly pills. Even if they get less menses, periods should definitely come, is widely believed.”
But skipping periods can also alleviate a sanitary burden on women. With a majority of Indian women lacking access to menstrual products, clean bathrooms and other sanitary facilities, making periods an option can help reduce health risks for them. Young girls are also made to miss school and told to forego opportunities because of periods, an obstacle that skipping periods can obliterate from their lives.
Related on The Swaddle:
Are There Any Long-Term Side Effects of Birth Control Pills?
Despite the benefits, period suppression has some disadvantages that are difficult to ignore. First, the body takes some time to adjust to period-suppressing birth control. It takes two to three months to regularize the body’s hormones, and it can also lead to initial spotting, said Dr.Nadkarni. People can also experience slight weight gain, bloating and heaviness, due to water retention in the body, she said. In the case of hormonal implants, it is possible the person experiences breakthrough bleeding initially, which usually disappears with prolonged use, she added.
Period suppression can also hide underlying disorders made apparent by monthly menstruation, such as endometriosis. “Having periods is not a disease. But when they go wrong, they offer clues into disorders that require intervention. … Clinicians tend to wield synthetic hormones like a hammer, liberally prescribing the birth control pill for all kinds of pain — which is partly why serious diseases of the female organs such as endometriosis take an average of eight years to be diagnosed,” according to the Scientific American. Long-term use of birth control also poses certain risks; however, the research into birth control’s detrimental effects on a woman’s body is limited. If you haven’t had the HPV vaccine, then there is some evidence birth control hormones can aid the HPV virus in developing into precancerous cervical lesions. Long-term use of oral contraceptives can also increase the risk of getting breast cancer — by approximately 20% — and one study says the risk increases with the duration of contraceptive use. Prolonged birth control use after 35 is also not advisable, as increased doses of estrogen, one of the hormones in contraceptives, can elevate the risks for blood clots and heart attacks.
Before taking birth control to suppress periods, especially for longer durations, it is important to consult a gynecologist to evaluate any risks that might come with prolonged use.
Rajvi Desai is The Swaddle's Culture Editor. After graduating from NYU as a Journalism and Politics major, she covered breaking news and politics in New York City, and dabbled in design and entertainment journalism. Back in the homeland, she's interested in tackling beauty, sports, politics and human rights in her gender-focused writing, while also co-managing The Swaddle Team's podcast, Respectfully Disagree.
Related


Fasting Aids Weight Loss More by Suppressing Hunger Hormones Than by Burning Calories
