For most of us, the immune system works to protect us from bacteria, viruses, and other harmful pathogens. But for people with autoimmune conditions, the body’s white blood cells instead perceive other cells and tissues in the body to be a threat and attacks them. While some immune disorders, like allergies, can sometimes be treated, autoimmune conditions such as multiple sclerosis (MS) remain incurable.
Our research has shown that you can stop the immune system attacking the nerves – which is what happens in MS. We did this by giving the immune system ever-increasing doses of the same molecule that the immune system was attacking.
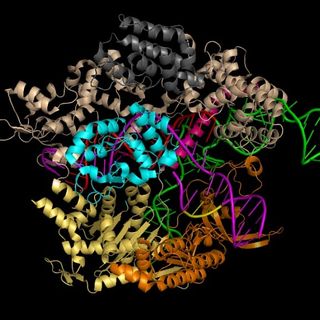
Now we’ve taken this research one step further to show how this process works inside the white blood cells that make up the immune system. Our team revealed the complex mechanisms that allow us to switch T cells (a type of white blood cell) from attacking the cells of autoimmune disease patients to protecting them. We learned how to make reactive T cells tolerant.
Related on The Swaddle:
Female Immune System Could Hold Key to Fighting Cancer, Autoimmune Disorders
Our T cells have evolved so that each one recognises different parts of the molecules made by pathogens (also known as antigens). When the T cells recognise antigens, the T cells start multiplying in order to attack the invaders. The T cells move from a resting state into a highly activated state by turning on immune response genes that help them attack pathogens.
When an infection is over, some of these T cells remain, giving lifelong immunity as memory T cells. They’re able to carry this lifelong memory by imprinting our chromosomes with triggers that allow immune response genes to be reactivated much faster.
In autoimmune diseases such as MS, Graves’ disease, and type 1 diabetes, the immune system gets it wrong. In MS, the T cells start to see myelin basic protein, a component of the external insulating coating that surrounds nerve cells, as an antigen. They attack the nervous system and, as a result, MS sufferers lose control over their muscles. Our research is trying to rectify this.
Weakening T cells
To help us understand this process, we focused on the T cells that specifically recognize myelin basic protein as an antigen. We found that over time these T cells became less reactive after they were exposed to gradually increasing doses of the myelin basic protein. This progressive exposure reprogrammed these T cells so that the signals telling the cells to attack the protein became weaker. This converted the T cells from attacking to protecting.
This switch could be explained by the fact that the immune system is regulated by two types of genes. One type tells the immune system to attack, while the other gene type silences the immune system to stop it going out of control.
We showed that when T cells are made tolerant, two of the most important genes that suppress the immune system were reprogrammed at the level of the chromosome to keep them more active. Repetitive exposure to the myelin basic protein imprinted a memory within these inhibitory genes. This allowed T cells to remember to inhibit the T cell receptor from sending attack signals when they encountered that same specific myelin basic protein fragment.
The end effect of turning on the inhibitory genes was to weaken the signals inside T cells that would normally turn on other genes that activate the immune system. That meant that the T cells stopped getting the signal telling them to attack nerve cells.
Related on The Swaddle:
Lupus: the Immune System Malfunction Science Is Yet to Decipher
Autoimmune diseases are currently treated using immunosuppressive drugs. The problem with this is that they suppress the whole immune system, making the patient prone to cancers and other infections. Trials using antigen therapy in patients with MS and Grave’s disease are ongoing, but results from short-term preliminary clinical trials showed both MS and Graves’ disease patients started to have improved health while the trials lasted.
One day we hope that antigen-based immunotherapy will be able to deliver major benefits for all types of autoimmune disease. By detailing the complex mechanisms that control the fate of self-reactive T cells, we may have also opened the door for more specific therapies for these diseases.
This article is republished from The Conversation.