Scientists Are Employing 3D Printing to Devise Treatments for Breast Cancer
Scientists used 3D bioprinting or biofabrication, a method used in medical research to fabricate biological organs and tissues in the lab.
In the last few years, 3D printing has become an effective and efficient piece of technology. It is being used in a range of industries. NASA, for instance, is looking at using 3D-printing technology to minimize food wastage in space. Elsewhere, fashion companies are building both prototypes and actual garments using 3D printers. In Hong Kong, 3D-printing technology is being used to rebuild coral reefs.
But one of the most important uses of the 3D-printing technology, perhaps, has been its application in medical research. A group of scientists has used 3D printing to make a new breakthrough in breast cancer research and treatment.
Breast cancer is the leading type of cancer in women worldwide, accounting for close to a fourth of all cancer cases. Although treatment methods have severely improved conditions, even in 2020 around 2.3 million individuals were affected by breast cancer, and close to 7,00,000 people died of it. This makes it one of the foremost causes of mortality worldwide, and an area of continuous research in medical science. During the same time in India, breast cancer along with cervical cancer accounted for close to 40% of total cancer cases in women. More than two lakh Indian women were diagnosed with breast cancer in 2020, of which more than 76000 lost their lives.
Researchers are constantly hoping to devise new methods of detecting and treating breast cancer. In pursuance of that, the current research — findings of which were published earlier this month and late last month in the journal Advanced Functional Materials and the journal Biofabrication respectively — is another step in that direction. In the present study, the scientists used 3D bioprinting or biofabrication, a method used in medical research to fabricate biological organs and tissues in the lab, to create breast cancer tumors, and then test treatment methods on these bioprinted tumors.
“We’ve developed a tool that serves as a clinical test platform to safely and accurately evaluate experimental therapies. It is also a research platform for immunologists and biologists to understand how the tumor grows, how it interacts with human cells, and how it metastasizes and spreads in the body,” explained co-author Ibrahim Ozbolat, highlighting the significance of their research.
Related on The Swaddle:
Breast Cancer Spreads More Aggressively at Night, Finds New Study
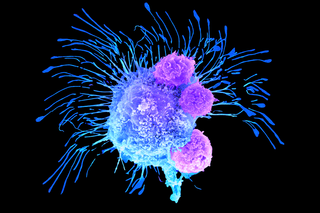
On observing the tumors reacting to doxorubicin, a common chemotherapeutic drug used for treating breast cancer, the scientists affirmed that their models accurately represented breast cancer tumors. The scientists then proceeded to try immunotherapy — a method of cancer treatment that employs a patient’s own immune system to fight against cancer cells — to examine how effective it was against the bioprinted tumors.
“Essentially, immune cells of the patient are removed and gene-edited to be cytotoxic for cancer cells, then reintroduced into the patient’s bloodstream. Circulation is critical because the altered cells need to move around the body. With tumors, that kind of effective circulation doesn’t exist, so we built our model to try to better understand how tumors respond to immunotherapy,” noted Ozbolat, a biomedical engineering professor at the Pennsylvania State University, USA.
The researchers used Chimeric Antigen Receptor T cells (CAR-T cells) to test the effectiveness of immunotherapy in treating breast cancer. After 72 hours of circulating these CAR-T cells in the bioprinted tumors, the scientists observed that they generated a positive immune response and were fighting the cancer cells in the tumor. Thus, the researchers were successful in employing immunotherapeutic methods for treating cancer present in tumors, which was earlier thought to be much more difficult due to the lack of effective circulation. This opens up new possibilities for the treatment of breast tumors.
The scientists emphasize in their research that their model, although made from human cells, is a simplified version of a breast cancer tumor, and that the complexities need to be accounted for in further experiments. “There are many details that exist in the native microenvironment that we aren’t able to replicate, or even consider replicating. We are aiming for simplicity within complexity. We want to have a fundamental understanding of how these systems work — and we need the growth process to be streamlined, because we don’t have time to wait for tumors to grow at their natural pace,” Ozbolat says.
Bioprinted models, built accurately, can open up new methods of testing and devising treatment methods for cancer. That way, they can serve as a platform for trying novel forms of treatment without involving or putting human subjects at risk. Moreover, since these models can be designed according to the scientists’ preferences, they can also provide a larger range and ground for more effective and accurate testing. “This is an important step in understanding the intricacies of the disease, which is essential if we are going to develop novel therapeutics and targeted therapies against cancer,” Ozbolat said
Amlan Sarkar is a staff writer at TheSwaddle. He writes about the intersection between pop culture and politics. You can reach him on Instagram @amlansarkr.
Related


Can We Erase Traumatic Memories?